Clinical Outcomes and Risk Factors for Delayed or Slow Graft Function in an Adult, Urban Renal Transplant Population
University of Illinois at Chicago, Chicago, IL
Meeting: 2019 American Transplant Congress
Abstract number: C75
Keywords: Biopsy, Graft function, Kidney
Session Information
Session Name: Poster Session C: Kidney Complications: Late Graft Failure
Session Type: Poster Session
Date: Monday, June 3, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: Delayed graft function (DGF) and slow graft function (SGF) are shown to be associated with higher risk of rejection and suboptimal allograft function over time. DGF is an independent risk factor for the development of acute rejection. However, the clinical implications of SGF after renal transplant (RTx) are less defined. The purpose of this study is to evaluate differences in short- and long-term transplant outcomes post-RTx by DGF, SGF, or immediate graft function (IGF) in an adult, urban population.
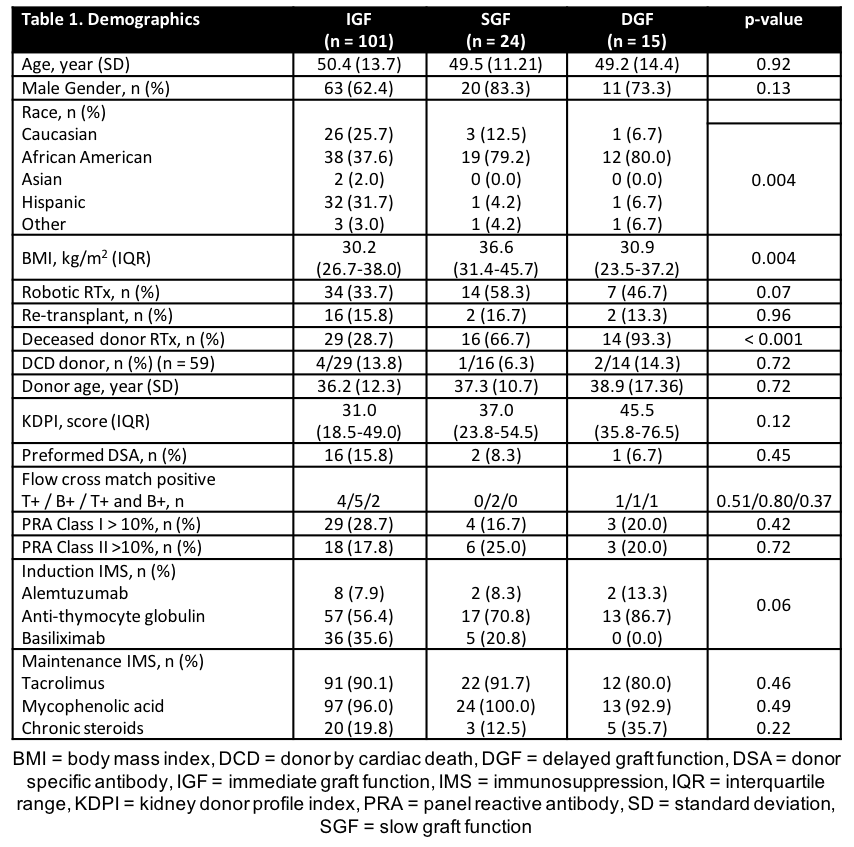
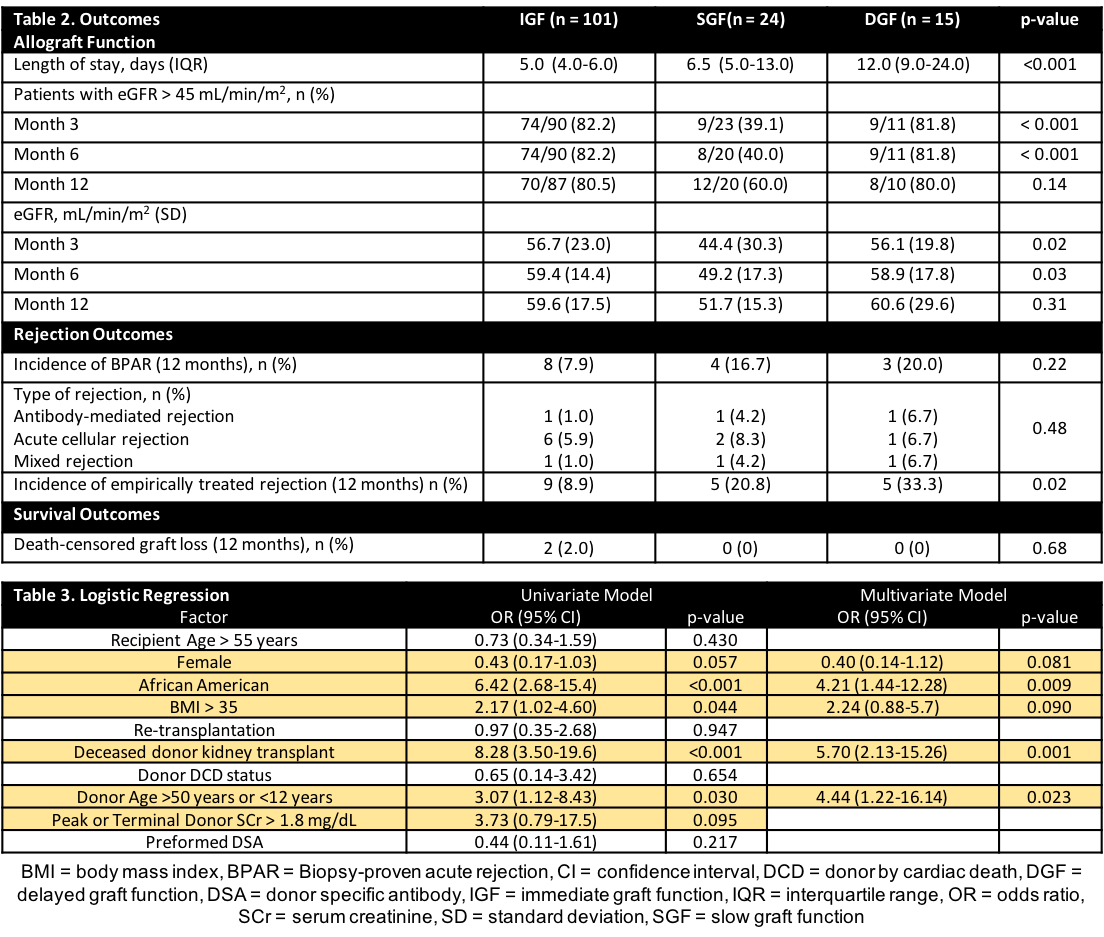
*Methods: Adult RTx recipients from 1/2015 – 10/2017 were assessed. DGF was defined as need for dialysis before post-operative day (POD) 7. SGF was defined by <50% decrease in serum creatinine (SCr) from pre-RTx SCr or SCr ≥ 3.00 mg/dL by POD7. The primary outcome was incidence of patients with an estimated glomerular filtration rate (eGFR) ≥ 45mL/min/1.73m2 at 3 months post-RTx. Univariate and multivariate logistic regression was performed to identify risk factors for acute-tubular necrosis (ATN) post-RTx.
*Results: 140 patients were analyzed. A majority of patients were African American (49.3%), male (67.1%), and received living RTxs (57.9%) (Table 1). Patients with SGF and DGF had a significantly longer length of stay (LOS) compared to those with IGF (p<0.001). Mean eGFR was highest in IGF patients at 3 months (p <0.001); however, eGFR was similar at 12 months (p=0.14). Incidence of biopsy-proven rejection (BPAR) was not significant (p=0.22). Incidence of empirically treated rejection was significantly different (DGF 33.3% vs SGF 20.8% vs IGF 8.9%, p=0.02). Death-censored graft loss at 12 months was similar (p=0.68) (Table 2). In multivariate analysis, African American race (OR=4.21, p =0.009), deceased donor RTx (DDRT) (OR=5.70, p = 0.001), and donor age (OR=4.44, p=0.23) significantly increased the risk for immediate post-RTx ATN (Table 3). Obesity did not impact ATN risk.
*Conclusions: Immediate post-RTx ATN (i.e. DGF and SGF) was associated with longer LOS, poorer acute allograft function. However, at 12 months, BPAR, allograft function, and graft survival were similar. Race, DDRT, and donor age increased risk for ATN development.
To cite this abstract in AMA style:
Tejani K, Hajjiri Z, Benedetti E, Lichvar A. Clinical Outcomes and Risk Factors for Delayed or Slow Graft Function in an Adult, Urban Renal Transplant Population [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/clinical-outcomes-and-risk-factors-for-delayed-or-slow-graft-function-in-an-adult-urban-renal-transplant-population/. Accessed February 15, 2026.« Back to 2019 American Transplant Congress