Changes to Adult Heart Allocation Improve Candidate Stratification
1Research, United Network for Organ Sharing, Richmond, VA, 2Mayo Clinic, Rochester, MN, 3Baylor University Medical Center, Dallas, TX
Meeting: 2021 American Transplant Congress
Abstract number: 103
Keywords: Allocation, Heart, Heart/lung transplantation, Monitoring
Topic: Clinical Science » Public Policy » Non-Organ Specific: Public Policy & Allocation
Session Information
Session Name: Potpourri of Public Policy and Allocation
Session Type: Rapid Fire Oral Abstract
Date: Sunday, June 6, 2021
Session Time: 4:30pm-5:30pm
 Presentation Time: 4:30pm-4:35pm
Presentation Time: 4:30pm-4:35pm
Location: Virtual
*Purpose: Historically, heart allocation has been driven by waitlist (WL) mortality rather than post-transplant survival. On 10/18/2018 the Organ Procurement and Transplantation Network (OPTN) implemented modifications to the adult heart allocation system intended to better stratify the most medically urgent candidates by WL mortality.
*Methods: The impact of changes to the adult heart allocation system were assessed by comparing cohorts of WL additions and candidates transplanted pre (04/18/17-10/17/18) and post (10/18/18-04/17/20) implementation. WL mortality, median time to transplant, transplant rates and six-month survival were compared between medical urgency statuses, status criteria and era. Fine-Grey competing risks and unadjusted Kaplan Meier methods were used to estimate median days to transplant and 6-month patient survival, respectively.
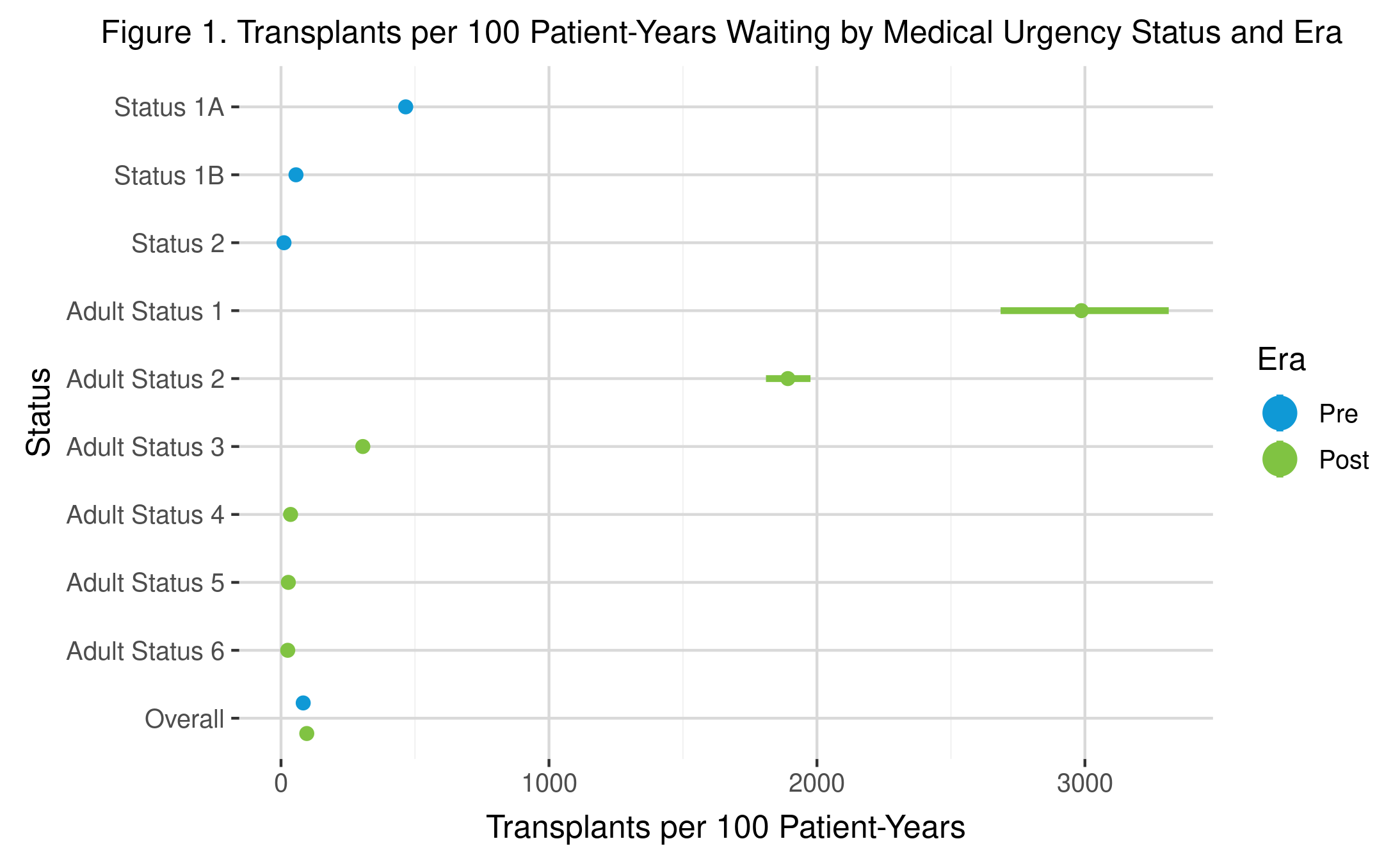
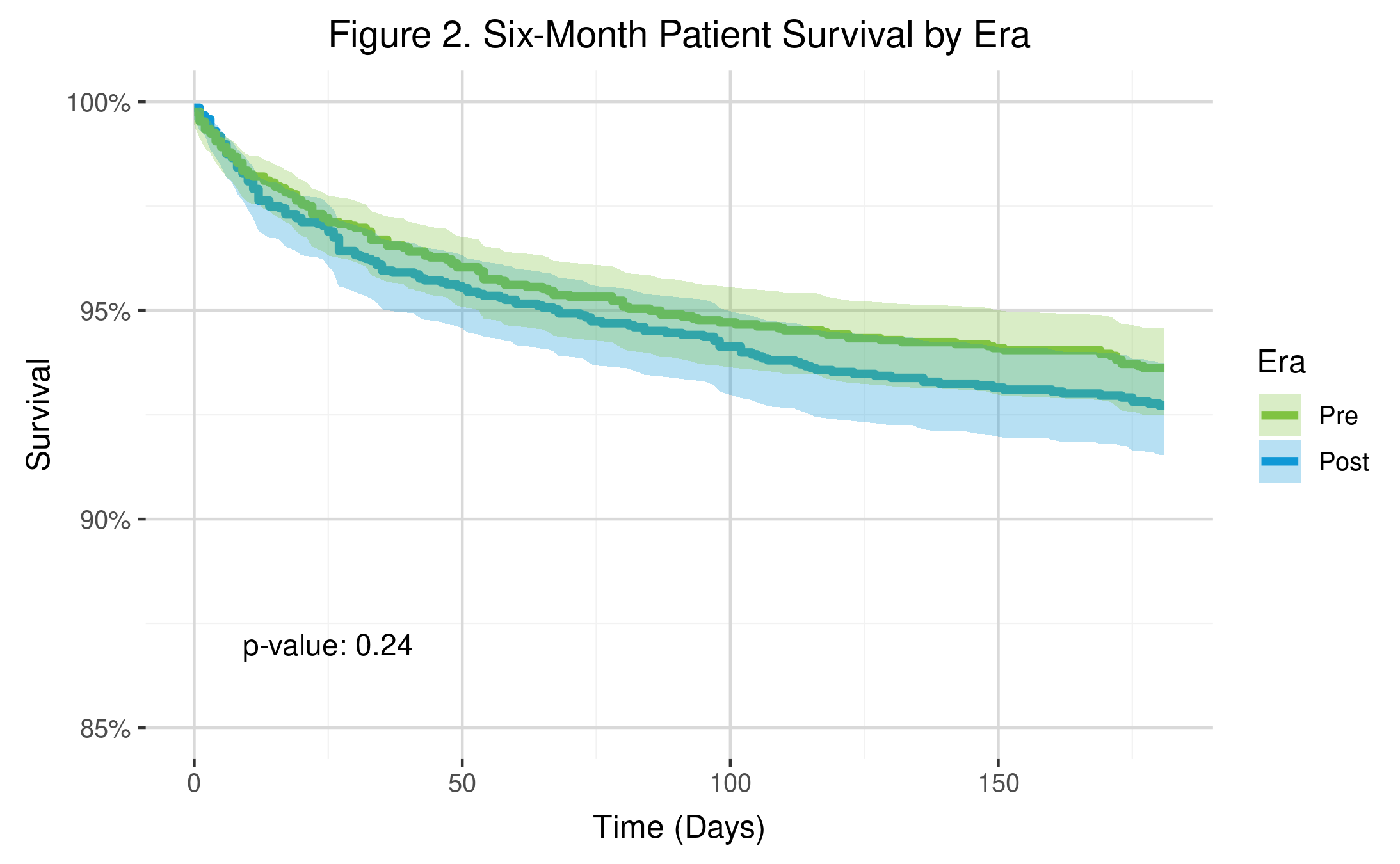
*Results: WL mortality was significantly higher for Status 1 vs. Status 2 and for Status 2 vs. Status 3 candidates. Criteria within medical urgency statuses had similar WL mortality rates. Median days to transplant decreased pre- to post-implementation (Mpre= 224, Mpost= 105) with higher statuses having shorter wait times (Status 1 Mpost= 5, Status 2 Mpost= 10, Status 3 Mpost= 28 days). Median time to transplant varied across criteria within statuses, with a maximum within-status difference of 226 days. Transplant rates were significantly higher for the most medically urgent candidates compared to each subsequent status (Status 1: 2987 [2685, 3313]; Status 2 1891 [1810, 1976]; Status 3: 305 [286, 326]; Transplants per 100 patient years). Six-month patient survival did not differ between eras (pre=93.6%, post=92.7%; p=0.24).
*Conclusions: Overall, the implementation of the new adult heart allocation policy resulted in better stratification of the most medically urgent heart candidates according to risk of death on the WL with decreased median wait times, higher transplant rates and no observed adverse effect on 6-month patient survival.
To cite this abstract in AMA style:
Bradbrook K, Lindblad K, Goff RR, Daly R, Hall S. Changes to Adult Heart Allocation Improve Candidate Stratification [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/changes-to-adult-heart-allocation-improve-candidate-stratification/. Accessed February 18, 2026.« Back to 2021 American Transplant Congress