Body Mass Index (BMI) Mismatch in Deceased Kidney Donation Is an Independent Risk Factor for Graft Failure
1Nephrology, Charite Universitaetsmedizin, Berlin, Germany
2Urology, Charite Universitaetsmedizin, Berlin, Germany.
Meeting: 2015 American Transplant Congress
Abstract number: A138
Keywords: Graft survival, Kidney transplantation, Obesity, Outcome
Session Information
Session Name: Poster Session A: Kidney Candidate Issues and Outcomes
Session Type: Poster Session
Date: Saturday, May 2, 2015
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Exhibit Hall E
Introduction
The influence of this BMI-mismatch in deceased kidney donors and their recipients on graft survival is so far not well characterized.
Methods
Retrospective long-term observational study of a cohort of 549 patients who received a kidney from deceased donors 2000-2013. Demographics, clinical data and long-term outcome over maximal 14 years post-transplant were assessed. Mean follow up was 6.4±3.3 years. The cohort was further categorized in two groups according to the median BMI-mismatch: patients who received a graft from a donor with a BMI which differed ≥4 kg/m2 (n=265) and patients with a similar BMI category (mismatch <4 kg/m2, n=284).
Results
There was a significant association of graft loss with BMI-mismatch, HLA-mismatch, donor age and recipient BMI. Donor and recipient height or weight, mismatch in height, mismatch in weight, donor BMI and recipient age showed no significant association with graft loss. In the multivariate analysis BMI-mismatch was identified as an independent predictor for allograft loss. Other independent risk factors in this analysis were pre-transplant recipient BMI and donor age. HLA-mismatch did not reach significance level in this analysis (table 1).
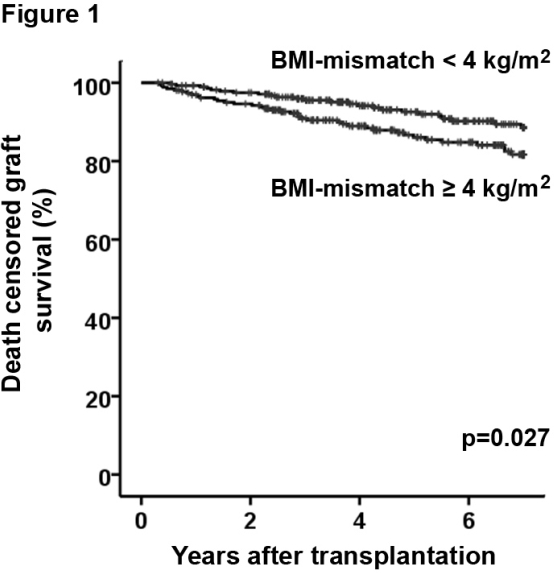
The group with a BMI-mismatch ≥4 kg/m2 showed significantly lower predicted graft survival (7 years after transplantation 0.82 vs 0.89, log rank p=0.027) (figure 1). Within the group of patients with a BMI-mismatch ≥4 kg/m2 recipients who received a graft from a donor with a lower BMI were prone to a further elevated risk vs. donors with a higher BMI (0.78 vs. 0.84). The baseline characteristics including donor and recipient age, sex, height, weight, cause of ESRD, HLA-mismatches and number of prior kidney transplantations did not differ significantly.
Conclusions
BMI-mismatch in deceased kidney donors and their recipients is an independent risk factor for kidney allograft loss.
| Table 1: Factors associated with graft loss (multivariate analysis) | |||
|---|---|---|---|
| Variable | HR | p | |
| BMI-mismatch per 1 kg/m2 | 1.06 | 0.009 | |
| Donor age per 1 y | 1.05 | <0.001 | |
| HLA-mismatches per 1 | 1.16 | 0.063 | |
| Recipient BMI per 1 kg/m2 | 1.05 | 0.046 | |
To cite this abstract in AMA style:
Staeck O, Khadzhynov D, Mahn M, Budde K, Fuller F, Halleck F. Body Mass Index (BMI) Mismatch in Deceased Kidney Donation Is an Independent Risk Factor for Graft Failure [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/body-mass-index-bmi-mismatch-in-deceased-kidney-donation-is-an-independent-risk-factor-for-graft-failure/. Accessed July 18, 2025.« Back to 2015 American Transplant Congress
