Beyond CPRA: Identifying Sensitized Kidney Candidates with Markedly Low Access to Transplant
1UNOS, Richmond, VA, 2Hansa Biopharma AB, Lund, Sweden, 3Immucor, Norcross, GA
Meeting: 2022 American Transplant Congress
Abstract number: 264
Keywords: Cadaveric organs, Histocompatibility, Kidney transplantation, Sensitization
Topic: Clinical Science » Public Policy » 21 - Non-Organ Specific: Public Policy & Allocation
Session Information
Session Name: Non-Organ Specific: Public Policy & Allocation
Session Type: Rapid Fire Oral Abstract
Date: Monday, June 6, 2022
Session Time: 3:30pm-5:00pm
 Presentation Time: 4:00pm-4:10pm
Presentation Time: 4:00pm-4:10pm
Location: Hynes Room 311
*Purpose: The Kidney Allocation System (KAS) improved the rates of transplantation in highly sensitized (HS) patients. However, a subset of HS patients remain at a disadvantage. This analysis examines parameters beyond calculated panel reactive antibody (CPRA) that may impact an HS candidate’s access to deceased donor transplant.
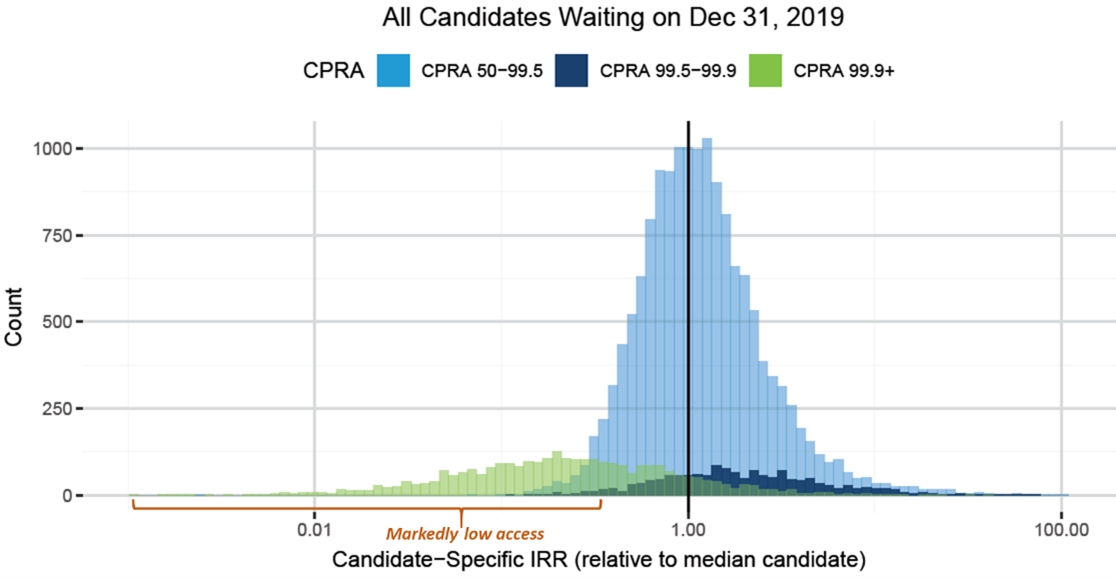
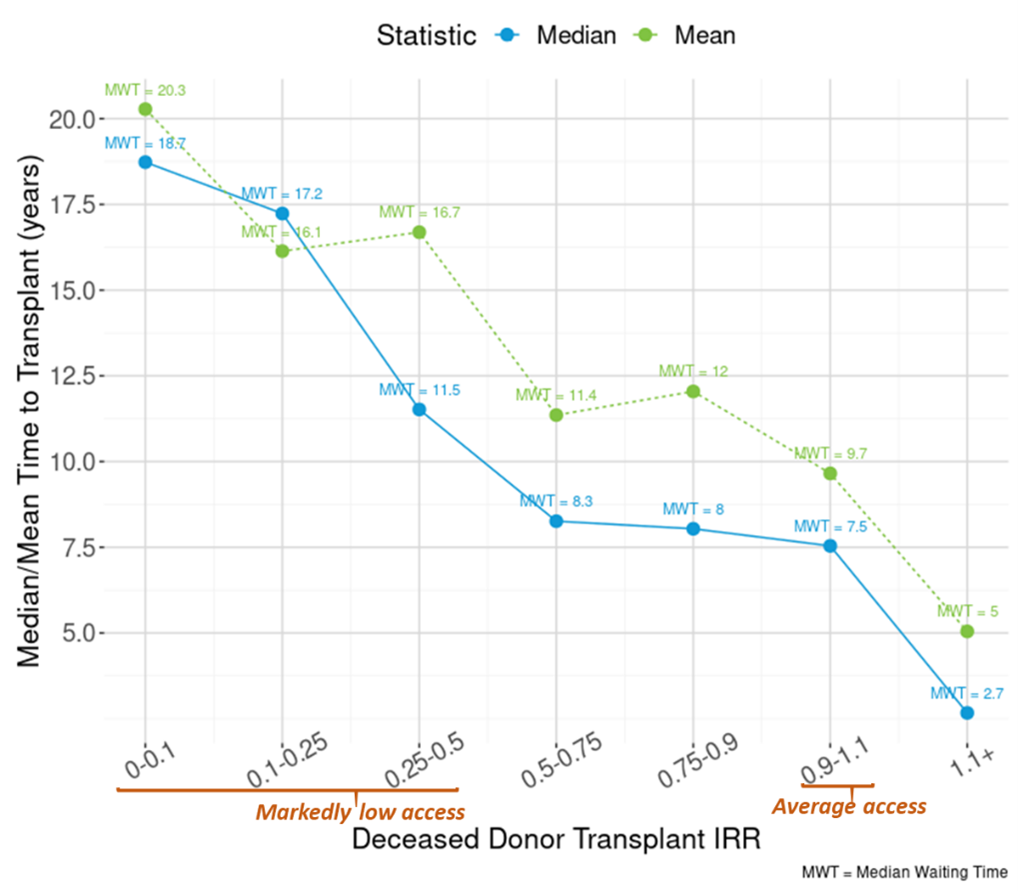
*Methods: The OPTN’s access to transplant score (ATS) framework was leveraged using Poisson rate regression to measure equity in access to deceased donor transplant on kidney-alone registrations in the OPTN database waiting at least one day from 04/01/2016-12/31/2019. Transplant rates were converted to incidence rate ratios (IRRs) by dividing predicted by median transplant rate for all registrations waiting on 12/31/2019. Local supply to demand ratios were included to account for geographic variation. Kaplan Meier survival was used to estimate median time to transplant by IRR.
*Results: At the start of 2020, the kidney waiting list consisted of 2,526 candidates with a CPRA of 99.9% or greater, a cohort demonstrated to have markedly lower than average access to transplant under KAS. An additional 4,080 less sensitized (CPRA 50-99.9%) candidates were also identified as having markedly lower than average access. These patients tended to have blood type O or B, Estimated Post-Transplant Survival Score (EPTS) 21-80%, diabetes, a prior transplant, unacceptable HLA DP-Beta antibodies (currently not included in CPRA determination), and low supply-to-demand ratio.
*Conclusions: Approximately 6,500 HS candidates on the kidney waiting list had markedly low access to deceased donor transplant due to sensitization in combination with other factors. Most of these candidates were predicted to receive transplants at 25% to 75% the rate of candidates with average access, which translates into approximately 4 to 7 years of additional waiting time. With an annual mortality risk of approximately 5% for candidates waiting for a kidney transplant, this added waiting time translated into a 19% (4 years) to 30% (7 years) increased risk of dying without a transplant. Recognizing the need for a multifactorial approach to identify these patients is a first step towards improved equity.
To cite this abstract in AMA style:
Bradbrook K, Maldonado A, Sjöholm K, Kjellman C, Lee J, Stewart D. Beyond CPRA: Identifying Sensitized Kidney Candidates with Markedly Low Access to Transplant [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/beyond-cpra-identifying-sensitized-kidney-candidates-with-markedly-low-access-to-transplant/. Accessed February 17, 2026.« Back to 2022 American Transplant Congress