Belatacept-Treated Patients Had Better Graft Survival at 7-Years Post-Transplant Compared With Cyclosporine-Treated Patients: Final Results from BENEFIT
1Univ of Calif, San Francisco
2Univ Hosp Bellvitge, Barcelona, Spain
3Univ Hosp and INSERM U563,IFR-BMT, Toulouse, France
4Baylor Univ Med Ctr, Dallas
5Sharp Memorial Hosp, San Diego
6Hôp de La Cavale Blanche, Brest, France
7BMS, Lawrenceville
8Emory Univ Transpl Ctr, Atlanta.
Meeting: 2015 American Transplant Congress
Abstract number: 515
Keywords: Graft survival, Immunosuppression, Kidney transplantation, Renal function
Session Information
Session Time: 8:30am-10:00am
 Presentation Time: 9:45am-10:00am
Presentation Time: 9:45am-10:00am
Location: Terrace Ballroom 1, 2, 3
Background: At 3yrs, improvement in renal function was seen in kidney transplant recipients treated with belatacept (bela) vs cyclosporine (CsA) in BENEFIT. Here we report 7yr results for all randomized pts from BENEFIT.
Methods: Pts were randomized to more (MI) or less intensive (LI) bela or CsA. All pts received basiliximab induction/MMF/CS. Outcomes were assessed for all randomized and transplanted pts at Yr 7. In a prospective, post hoc, exploratory analysis, time to death or graft loss was compared between treatment groups using a Cox regression analysis. HR estimates and 95% CIs are provided.
Results: BENEFIT included 666 pts in the bela MI (n=219), bela LI (n=226) and CsA (n=221) groups. Over 7yrs, there was a 41% risk reduction in death or graft loss for pts receiving bela MI or LI vs CsA (p=0.0306, MI vs CsA; p=0.0286, LI vs CsA). Mean cGFR (MDRD, in mL/min/1.73 m2) at Mo 84 was 74 for MI, 78 for LI and 51 for CsA. Freedom from death, graft loss or cGFR <30 was 85%, 86%, and 67% for MI, LI and CsA. Acute rejection was observed in 24% MI, 18% LI and 10% CsA pts. Rates of SAEs were similar across treatment groups (72% MI, 69% LI, 76% CsA). Incidence rates (per 100 person-yrs) were similar across MI, LI and CsA, respectively, for fungal infections (7.8, 6.7, 7.6) viral infections (16.2, 14.2, 15.7) and malignancies (2.0, 1.7, 2.6). PTLD occurred in 3 MI (1 EBV+ [rate per 100 person-yrs, 0.09], 2 EBV- [1.50]), 2 LI (2 EBV+ [0.16]) and 2 CsA pts (1 EBV+ [0.10], 1 EBV-[0.61]). All PTLD cases in bela-treated pts occurred before Mo 24.
Conclusions: In this analysis of the final 7yr results from BENEFIT, bela-treated pts had better graft survival and renal function than CsA-treated pts. The bela safety profile was consistent with previous reports. 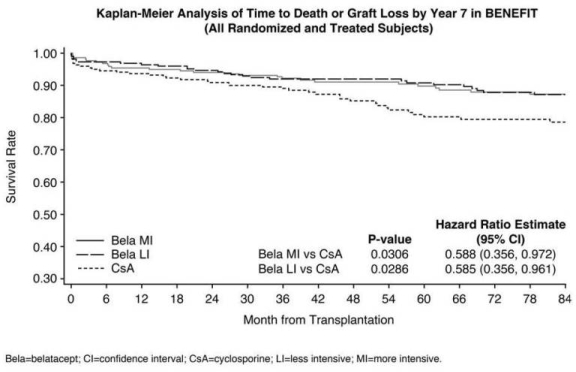
To cite this abstract in AMA style:
Vincenti F, Grinyó J, Rostaing L, Rice K, Steinberg S, Moal M, Polinsky M, Meier-Kriesche U, Larsen C. Belatacept-Treated Patients Had Better Graft Survival at 7-Years Post-Transplant Compared With Cyclosporine-Treated Patients: Final Results from BENEFIT [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/belatacept-treated-patients-had-better-graft-survival-at-7-years-post-transplant-compared-with-cyclosporine-treated-patients-final-results-from-benefit/. Accessed July 12, 2025.« Back to 2015 American Transplant Congress
