Arterial Hypertension After Renal Transplantation in Pediatric Patients: An Analysis of CERTAIN Registry.
R. Sugianto,1 E. Wühl,2 B. Schmidt,1 K. Krupka,2 B. Höcker,2 B. Tönshoff,2 A. Melk.1
1Children's Hospital, Hannover Medical School, Hanover, Germany
2Division of Pediatric Nephrology, University of Heidelberg, Heidelberg, Germany.
Meeting: 2016 American Transplant Congress
Abstract number: B231
Keywords: Kidney, Kidney transplantation, Multicenter studies, Post-transplant hypertension
Session Information
Session Name: Poster Session B: Kidney: Cardiovascular and Metabolic
Session Type: Poster Session
Date: Sunday, June 12, 2016
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Halls C&D
Background
Our study aimed to describe the prevalence of hypertension & blood pressure (BP) control as well as influencing factors in pediatric renal transplant patients.
Method
Casual BP values, number and type of AH medication were analyzed in 259 pediatric renal transplant patients from the CERTAIN Registry, for which data entries were available at discharge, at 1. 2 and 3 year follow-up visit. Patients were classified as “normotensive” (if untreated and normotensive), “controlled hypertensive (HT)” (if treated and normotensive), “uncontrolled HT” (if treated and still HT) and “untreated HT” (if untreated and HT).
Results
At discharge 17% were normotensive, 27% controlled HT, 46% uncontrolled HT, and 10% untreated HT. At 1(3) years posttransplant 23(24)% were normotensive, 39(39)% controlled HT, 31(27)% uncontrolled HT and 9(9)% untreated HT (Figure 1a).
At 3 years, 25% of the patients were treated with single medication, 24% with a combination of two, and 13% with three to five AH agents. The pattern of drugs used changed over time: At discharge calcium antagonists (40%) and diuretics (32%) were most commonly used, whereas by 3 years posttransplant RAAS Blockers (46%) and calcium-antagonists (35%) was the most commonly used drugs (Figure 1b)
In the mixed model analysis, male gender, younger age higher BMI, steroid dose and antihypertensive treatment were significantly associated with an increased risk of higher systolic BP. There was a tendency towards a positive correlation with CNI through levels and towards a negative correlation with mTOR inhibitor use.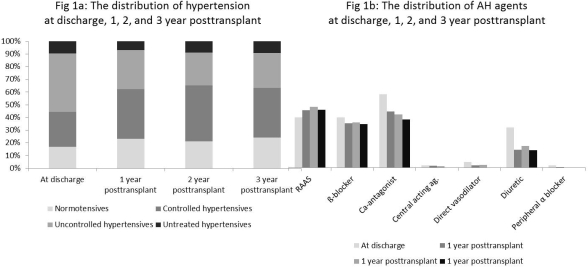
Conclusion
Arterial hypertension was present in more than a third of patients by 3 years after transplantation. In this cohort most patients (70%) were consistently under AH treatment with the need of multiple drugs. The use of AH drugs shifted from calcium-antagonists and diuretics immediately posttransplant to RAAS blockers and calcium-antagonists later on. Gender, age, BMI and steroid dose contributed significantly to higher BP levels.
CITATION INFORMATION: Sugianto R, Wühl E, Schmidt B, Krupka K, Höcker B, Tönshoff B, Melk A. Arterial Hypertension After Renal Transplantation in Pediatric Patients: An Analysis of CERTAIN Registry. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Sugianto R, Wühl E, Schmidt B, Krupka K, Höcker B, Tönshoff B, Melk A. Arterial Hypertension After Renal Transplantation in Pediatric Patients: An Analysis of CERTAIN Registry. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/arterial-hypertension-after-renal-transplantation-in-pediatric-patients-an-analysis-of-certain-registry/. Accessed July 18, 2025.« Back to 2016 American Transplant Congress
