Allo-Sensitization is Increased in Liver Transplant Recipients Following Ischemia-Reperfusion Injury
UCLA, Los Angeles, CA
Meeting: 2022 American Transplant Congress
Abstract number: 908
Keywords: Alloantibodies, HLA matching, Inflammation, Oxidant stress
Topic: Clinical Science » Organ Inclusive » 69 - Non-Organ Specific:Organ Preservation/Ischemia Reperfusion Injury
Session Information
Session Name: Non-Organ Specific: Organ Preservation/Ischemia Reperfusion Injury
Session Type: Poster Abstract
Date: Saturday, June 4, 2022
Session Time: 5:30pm-7:00pm
 Presentation Time: 5:30pm-7:00pm
Presentation Time: 5:30pm-7:00pm
Location: Hynes Halls C & D
*Purpose: Recipient sensitization to donor HLA antigens remains an important clinical problem in transplantation, leading to increased wait times to find a compatible donor and increased risk of acute and chronic cellular and antibody-mediated rejection. Given that a significant proportion of transplant candidates are allosensitized at the time of transplantation, this raises the question whether the activity of alloreactive cells present at the time of transplant potentiates IRI, or if IRI enhances the generation of donor alloreactive cells which then mediate graft rejection and lower long-term graft outcome. Here, we examine the influence of IRI on allo-immunity and the role of pre-existing allo-immunity on exacerbation of IRI.
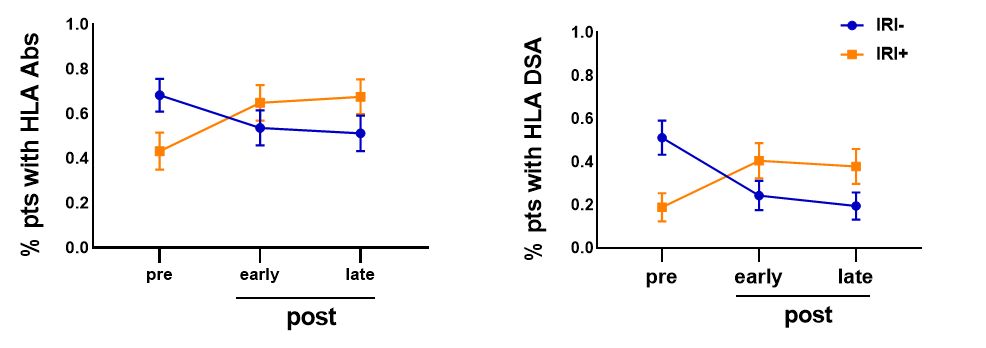
*Methods: We evaluated the production of donor-specific HLA class I and class II antibodies (DSA) pre- and at two timepoints post-transplant (early=within the first 3 months, and late=between 4 months and 2 years post-transplant) in OLT recipients with or without biopsy-proven IRI (n=78; IRI-=37, IRI+=41) using single antigen bead-based HLA antibody testing and intermediate resolution HLA typing (One Lambda).
*Results: OLT recipients who were pre-sensitized to HLA antigens prior to transplant were mostly protected from IRI, with 68% of IRI- patients being pre-sensitized compared to only 43% of IRI+ patients. There was also a significant decrease in the number of IRI- patients producing HLA antibodies early post-transplant, which further decreased late post-transplant. OLT recipients whose pre-sensitization was to HLA DSA were further protected from IRI with only 25% of DSA-producing patients having IRI complications. IRI+ patients who did not produce anti-HLA antibodies pre-transplant either had an early memory response that persisted through late testing or produced de novo antibodies late post-transplant. Importantly, IRI+ patients had a higher incidence of producing antibodies specific to the donor-allograft than IRI- patients at both acute and chronic AMR timepoints.
*Conclusions: Our data reveal that OLT recipients who are pre-sensitized to HLA antigens, particularly if they are donor-specific, are protected from IRI in the liver, an immunologically tolerant organ. Conversely, recipients who are not producing antibodies to HLA pre-transplant are significantly more likely to produce DSA to the mismatched HLA antigens carried by their transplanted allograft. As such, an increased frequency of post-transplant monitoring of liver transplant recipients without baseline pre-sensitization should be considered.
To cite this abstract in AMA style:
Sosa RA, Terry AQ, Yin Y, Naini BV, Kaldas FM, Busuttil RW, Gjertson DW, Kupiec-Weglinski JW, Reed EF. Allo-Sensitization is Increased in Liver Transplant Recipients Following Ischemia-Reperfusion Injury [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/allo-sensitization-is-increased-in-liver-transplant-recipients-following-ischemia-reperfusion-injury/. Accessed March 8, 2026.« Back to 2022 American Transplant Congress