Aligning Pediatric Waiting List and Post-Transplant Outcomes with the Adult Lung Allocation Score
1SRTR, Minneapolis, MN, 2Univ of Washington, Seattle, WA, 3Cleveland Clinic, Cleveland, OH, 4UNOS, Richmond, VA
Meeting: 2021 American Transplant Congress
Abstract number: 490
Keywords: Allocation, Lung, Outcome, Pediatric
Topic: Administrative » Quality Assurance Process Improvement & Regulatory Issues
Session Information
Session Name: Quality Assurance Process Improvement & Regulatory Issues
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: Lung allocation is moving toward a continuous distribution framework (CDF), with components for waitlist (WL) urgency and post-transplant (PT) survival, as computed in LAS. Candidates aged 0-11 years are excluded from LAS models and classified as Priority I (more urgent) or II. We computed expected WL and PT survival in this cohort to be used in the CDF to align with candidates aged ≥12 years who receive a lung allocation score (LAS).
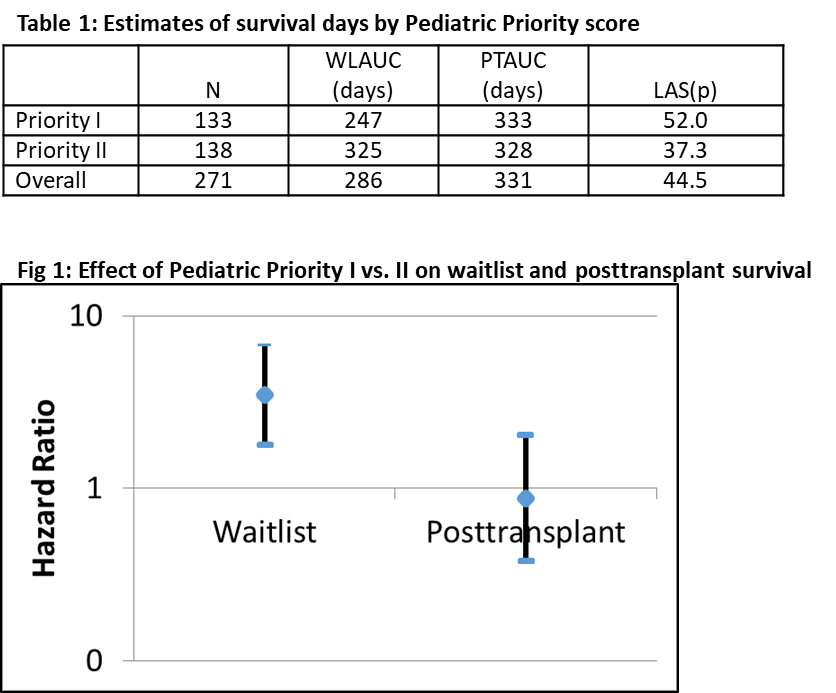
*Methods: We estimated predicted number of WL survival days within a year (WLAUC) and predicted number of PT survival days within a year (PTAUC) for Priority I and II candidates. Model cohorts included candidates and recipients aged 0-11 years from September 12, 2010 to January 31, 2019. WL follow-up was censored on the earliest of 1 year after joining the cohort; removal from the WL; January 31, 2020; or the candidate’s 12th birthday. Outcome was 1-year WL survival. PT follow-up was censored at 1-year PT. Outcome was 1-year PT survival. We fit Cox proportional hazards models, each with one covariate: Priority I vs. II. Each model generated a baseline survival function and an estimate associated with Priority I. From these, we computed the WLAUC and PTAUC for Priority I and II. We computed LAS(p) as a function of WLAUC and PTAUC, similar to LAS.
*Results: The WL cohort included 271 candidates, 54 (19.9%) of whom died waiting. Among 136 recipients, 51 (18.8%) died within 1 PT year. About half of patients (49.1%) were Priority I at cohort entry, and 58.1% were Priority I at transplant. Priority I was a risk factor for 1-year WL death but not 1-year PT death (Figure). Priority I and II patients were predicted to live 247 and 325 days, respectively, on the WL and 333 and 328 days PT. Priority I and II patients had effective median LAS(p) of 52.0 and 37.3, respectively (Table).
*Conclusions: Pediatric Priority can be aligned with LAS to allow pediatric patients to receive points for WL urgency and PT survival in a CDF. Pediatric priority is associated with WL mortality but not PT mortality.
To cite this abstract in AMA style:
Skeans M, Wey A, Lease E, Lehr C, Alcorn J, Goff R, Stewart D, Valapour M. Aligning Pediatric Waiting List and Post-Transplant Outcomes with the Adult Lung Allocation Score [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/aligning-pediatric-waiting-list-and-post-transplant-outcomes-with-the-adult-lung-allocation-score/. Accessed February 16, 2026.« Back to 2021 American Transplant Congress