Acute Liver Failure Etiology is an Independent Predictor of Waitlist Outcome Accounting for Severity of Illness in a National Cohort
University of Pennsylvania, Philadelphia, PA
Meeting: 2020 American Transplant Congress
Abstract number: C-161
Keywords: Liver failure, Liver transplantation, Survival, Waiting lists
Session Information
Session Name: Poster Session C: Liver: Recipient Selection
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Severity of illness and liver transplant (LT) waitlist outcome can differ according to acute liver failure (ALF) etiology. However, it is unknown whether ALF etiology predicts waitlist outcome independent of clinical parameters at the time of listing. This study evaluated waitlist outcomes among LT candidates with the four most common causes of ALF in the US: acetaminophen toxicity (APAP), drug induced liver injury not due to APAP (DILI), autoimmune hepatitis, and hepatitis B.
*Methods: All adults listed for primary LT between 2002-2019 with ALF due to APAP, DILI, autoimmune hepatitis and hepatitis B were identified in the United Network for Organ Sharing database. Waitlist outcomes included LT, removal due to death or deterioration, and spontaneous survivorship. Predictors of each outcome were evaluated using multivariable multinomial regression given the short time horizon from listing to waitlist removal. Models were adjusted for severity of illness at listing.
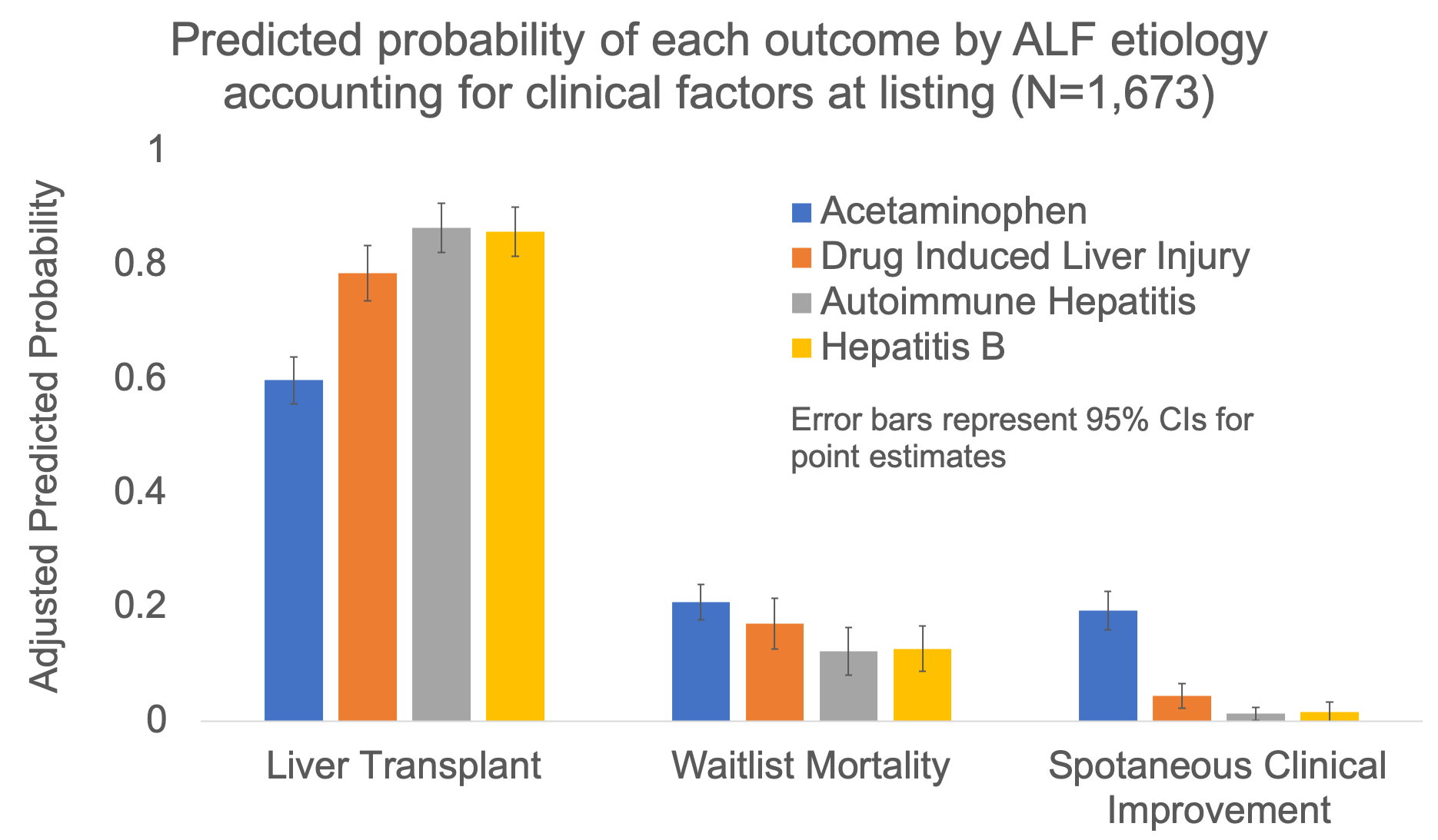
*Results: The final cohort included 1,691 patients: 765 (45.2%) with APAP, 292 (17.2%) with DILI, 315 (18.6%) with autoimmune hepatitis, and 319 (18.9%) with hepatitis B. APAP patients were sicker at listing, with 66% requiring mechanical ventilation (vs 37% DILI, 29% autoimmune, and 41% hepatitis B; p<0.001) and 14% requiring dialysis (vs 6% DILI, 4% autoimmune, 6% hepatitis B; p<0.001). Overall, 72.7% were transplanted, 17.3% died or became too sick, and 10% had clinical improvement. The adjusted relative risk ratios (aRRRs) for waitlist mortality compared to LT were lower for DILI, autoimmune hepatitis, and hepatitis B using APAP as reference: aRRR 0.65 (95% confidence interval [CI]: 0.43-0.96), 0.42 (95% CI: 0.26-0.67), and 0.44 (95% CI: 0.28-0.69) respectively (p<0.001). The aRRRs for spontaneous improvement compared to LT were also lower for non-APAP etiologies: aRRR 0.15 (95% CI: 0.08-0.28) for DILI, 0.04 (95% CI: 0.01-0.10) for autoimmune hepatitis, and 0.05 (95% CI: 0.01-0.16) for hepatitis B (APAP as reference; p<0.001). Adjusted predicted probabilities of each outcome by ALF etiology are shown in the Figure.
*Conclusions: ALF etiology is an independent predictor of waitlist outcome, even after adjusting for severity of illness and other clinical factors.
To cite this abstract in AMA style:
Wong NZ, Reddy KR, Bittermann T. Acute Liver Failure Etiology is an Independent Predictor of Waitlist Outcome Accounting for Severity of Illness in a National Cohort [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/acute-liver-failure-etiology-is-an-independent-predictor-of-waitlist-outcome-accounting-for-severity-of-illness-in-a-national-cohort/. Accessed July 3, 2025.« Back to 2020 American Transplant Congress