A Prognostic Biomarker to Estimate the Likelihood of Developing De Novo Donor Specific Antibody in Kidney Transplant Recipients
1Terasaki Research Institute, Los Angeles, CA, 2East Carolina University, Greenville, NC, 3Vidant Medical Center, Greenville, NC, 4Eastern Nephrology Associates, Greenville, NC
Meeting: 2019 American Transplant Congress
Abstract number: A130
Keywords: Alloantibodies, Kidney transplantation, Prediction models, Risk factors
Session Information
Session Name: Poster Session A: Biomarkers, Immune Monitoring and Outcomes
Session Type: Poster Session
Date: Saturday, June 1, 2019
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall C & D
*Purpose: Evaluation of human leukocyte antigen (HLA) mismatch at antibody epitope level rather than antigen level may explain better the impact of HLA mismatch on the risk of development of de novo donor-specific HLA antibody (dnDSA). To this end, we assessed the prognostic potential of mismatched HLA epitope loads (EpiL) and built machine learning models to estimate the probability of developing dnDSA within 2 years post-transplant.
*Methods: We obtained data on adult kidney transplant recipients (n = 804) who received a transplant at the East Carolina University between 3/15/1999 and 12/27/2015. Of these patients, those with missing data for any of the 14 variables tested or no HLA mismatch (n = 517) were removed from the analysis. EpiL for HLA-A, B, DRB1 and DQB1 were computed using E3 (Terasaki Research Institute). Recursive feature elimination with random forests was performed for variable selection. Selected risk factors were then used to train five machine learning algorithms. Bootstrapping was performed to estimate the variance of predicted probabilities. Model performance was measured using the receiver-operating characteristic (ROC) curve with c-statistic. Multiple model comparisons were done via DeLong’s test.
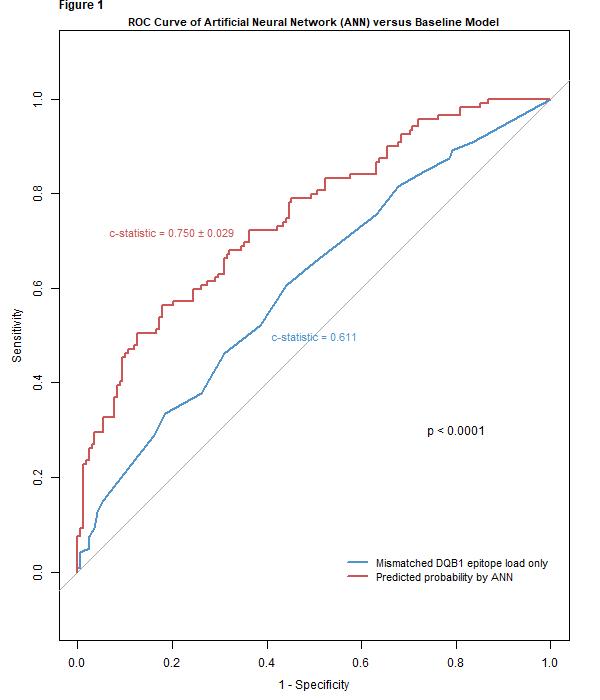
*Results: Of the 287 patients included in the analysis, 119 (41%) developed dnDSA within 2 years post-transplant. Nine potential risk factors for dnDSA development within 2 years were identified, of which HLA-DQB1 EpiL was given the highest variable importance score, suggesting that it is the most potent predictor of dnDSA. When trained with the selected variables, artificial neural network (ANN) had the highest prognostic performance with a c-statistic of 0.750 ± 0.029. Moreover, the ANN model performed significantly better (p < 0.0001) compared with the baseline model consisting of only mismatched DQB1 epitope load scores (Figure 1).
*Conclusions: We constructed a prognostic model, which enables us to identify patients at higher risk for development of dnDSA within the first 2 years post-transplant. Moreover, we found that among the variables tested, HLA-DQB1 EpiL had the most significant impact on the probability of developing dnDSA. Future efforts will focus on improving the current predictive system with additional data.
To cite this abstract in AMA style:
Kawakita S, Rebellato LM, Briley KP, Maldonado AQ, Haisch CE, Bolin P, Kendrick SA, Jones H, McLawhorn K, Leeser D, Jucaud V, Burnett V, Everly MJ. A Prognostic Biomarker to Estimate the Likelihood of Developing De Novo Donor Specific Antibody in Kidney Transplant Recipients [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/a-prognostic-biomarker-to-estimate-the-likelihood-of-developing-de-novo-donor-specific-antibody-in-kidney-transplant-recipients/. Accessed July 3, 2025.« Back to 2019 American Transplant Congress