A Novel Application of SRTR Data to Interrogate the Effects of HLA-DQ Mismatches in Kidney Transplantation
1Northwestern University, Chicago, IL, 2London School of Economics, London, United Kingdom, 3Cambridge University, Cambridge, United Kingdom, 4Cleveland Clinic, Cleveland, OH
Meeting: 2022 American Transplant Congress
Abstract number: 117
Keywords: Graft failure, Histocompatibility, HLA matching, Panel reactive antibodies
Topic: Clinical Science » Kidney » 47 - Kidney Complications: Immune Mediated Late Graft Failure
Session Information
Session Name: Kidney Complications: Chronic Antibody Mediated Rejection & Immune Mediated Late Graft Failure
Session Type: Rapid Fire Oral Abstract
Date: Sunday, June 5, 2022
Session Time: 5:30pm-7:00pm
 Presentation Time: 6:10pm-6:20pm
Presentation Time: 6:10pm-6:20pm
Location: Hynes Room 302
*Purpose: Single-center studies demonstrate de-novo HLA-DQ donor-specific antibodies (DSA) are the most common and pathogenic DSA. However, HLA-DQ is not accounted for in many kidney allocation schemes. Data in the Scientific Registry of Transplant Recipients (SRTR) do not include DSA and are therefore not amenable to directly study DQ DSA and transplant outcomes. We conceived a new approach looking at patients in the SRTR who returned to the kidney wait list after graft failure with new unacceptable antigens (UA) corresponding to the HLA type of the failed organ. This approach enables assessment of the differential role of HLA-DQ mismatches on graft loss and recipient sensitization.
*Methods: Adult patients in the SRTR who received a primary kidney transplant from 1/1/2010 – 3/1/2020 and were relisted after graft loss were included if they had donor/recipient typing and UA data at the HLA-A, B, C, DR and DQ loci along with cPRA before transplant and after relisting. Multiple linear regression was used to evaluate: 1) the probability of developing a new HLA UA corresponding to a mismatched donor antigen, 2) the increase in cPRA at relisting given development of a new donor-specific HLA UA and 3) the magnitude of these effects for HLA-DQ as compared to other loci. Models evaluating probabilities of new UA controlled for the effect of each HLA locus. Models evaluating cPRA controlled for other UA, HLA mismatches and waitlist time.
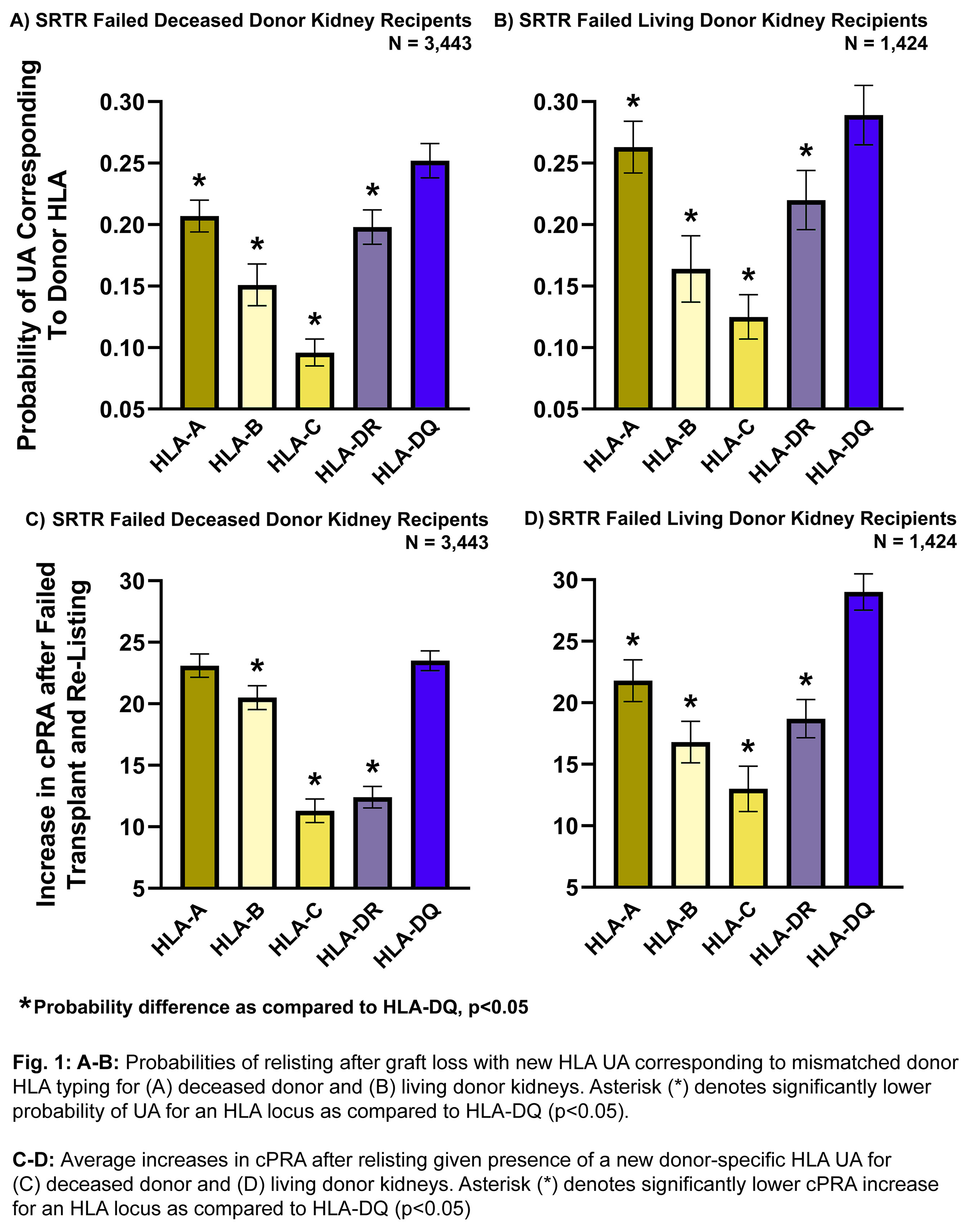
*Results: 3,443 deceased donor and 1,424 living donor recipients were included. The probability of an HLA-DQ mismatch producing a donor-specific DQ UA was 25.2% for deceased donor recipients and 28.9% for living donor recipients, significantly greater than every other HLA locus (Fig. 1A-B, p<0.05). The mean cPRA increase with a new DQ UA was 23.5% in deceased donor recipients and 29.0% in living donor recipients, significantly greater than all other HLA loci (Fig. 1C-D, p<0.05) except for HLA-A in deceased donor recipients (23.1%).
*Conclusions: This is the first study applying registry data to quantify the differential impact of HLA mismatches on generation of DSA (assessed based on UA at relisting) and on the likelihood of receiving a second kidney (measured as increase in cPRA). HLA-DQ mismatches have the highest probability of producing donor-specific UA after graft failure and result in the largest cPRA increases. These findings provide renewed impetus for consideration of HLA-DQ matching in kidney allocation algorithms.
To cite this abstract in AMA style:
Isaacson D, Gmeiner MW, Kosmoliaptsis V, Copley HC, Schold JD, Tambur AR. A Novel Application of SRTR Data to Interrogate the Effects of HLA-DQ Mismatches in Kidney Transplantation [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/a-novel-application-of-srtr-data-to-interrogate-the-effects-of-hla-dq-mismatches-in-kidney-transplantation/. Accessed February 18, 2026.« Back to 2022 American Transplant Congress