A Intention-to-Treat Analysis of 881 Consecutively Waitlisted Patients to Develop a Survival Benefit Model for Hepatocellular Carcinoma Liver Transplant Candidates
1Department of Surgery, University of California Los Angeles, Los Angeles, CA, 2Department of Medicine, Statistics Core, University of California Los Angeles, Los Angeles, CA
Meeting: 2022 American Transplant Congress
Abstract number: 1095
Keywords: Hepatocellular carcinoma, Liver transplantation, Multivariate analysis, Outcome
Topic: Clinical Science » Liver » 56 - Liver: Hepatocellular Carcinoma and Other Malignancies
Session Information
Session Name: Liver: Hepatocellular Carcinoma and Other Malignancies
Session Type: Poster Abstract
Date: Sunday, June 5, 2022
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: The current liver transplantation (LT) selection paradigm for hepatocellular carcinoma (HCC) patients ignores the variable risks of waitlist dropout and post-LT recurrence/death, with the same priority assigned to all eligible patients. We developed a novel risk model to identify HCC patients with the greatest survival benefit from LT.
*Methods: Clinicoradiologic and outcomes data of consecutively waitlisted HCC patients (2006-2015) at a single center were evaluated. Multivariate Fine and Gray competing-risk analysis identified independent predictors of HCC tumor progression, liver disease related waitlist dropout, and post-LT HCC recurrence, both at baseline and at the landmark 6 month time point. Survival benefit was defined as the predicted risk ratio of an adverse outcome following LT vs remaining on the waitlist, with patients stratified into 5 groups based on predicted 5-yr post-LT recurrence-free-survival (RFS) and survival benefit of LT > or < 25%.
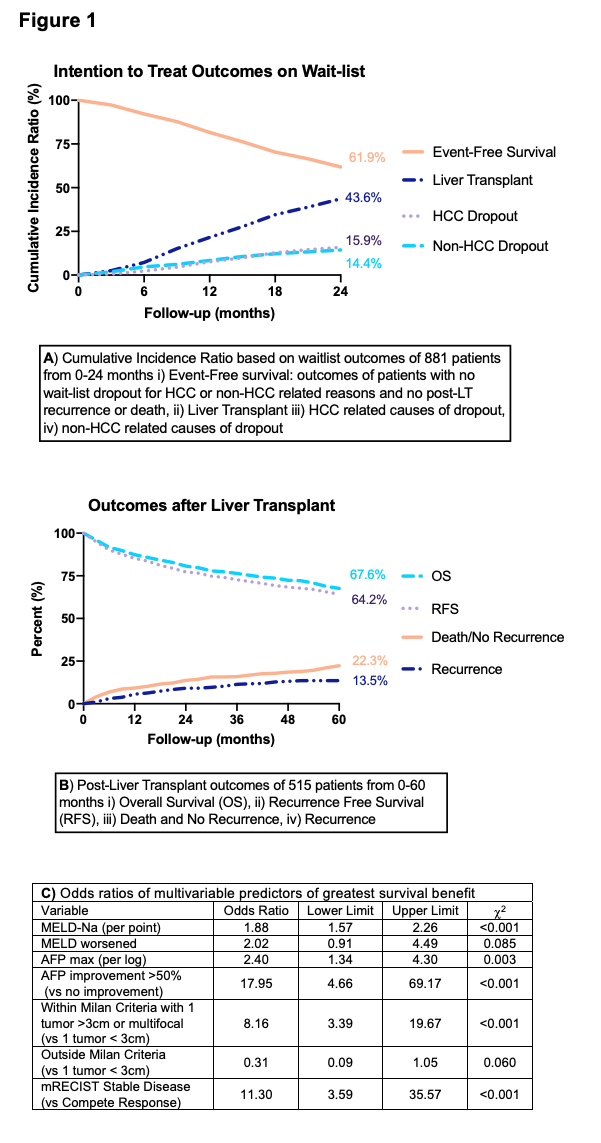
*Results: Of 881 HCC patients, 366 (41.5%) had wait-list dropout (median 16.0 months) and 515 (58.5%) underwent LT (median 15.6 months), with tumor progression (n=190) and non-HCC related liver complications (n=170) accounting for 51.9% and 46.4% of dropouts, respectively (Figure 1A). Of patients who underwent LT, 64 (12.4%) recurred and 102 (19.8%) died with no recurrence (Figure 1B, median follow-up 43.2 months). At baseline, AFP and radiologic size criteria independently predicted HCC-related dropout (c-stat 0.64), and MELD predicted liver related dropout (c-stat 0.65). At 6 months following diagnosis, AFP response to LRT, mRECIST, and radiologic size criteria improved HCC related dropout and post-LT recurrence model performance (c-stat 0.78 and 0.77, respectively). Model identified futile outcomes (< 50% RFS) in 23.7% of patients. In the remaining patients, multivariate predictors of greatest survival benefit (> 25% risk reduction of adverse event with LT vs waitlist) included MELD at baseline and change in MELD at 6 months, AFP max and AFP response, radiologic size criteria at baseline, and mRECIST response (Figure 1C).
*Conclusions: We report a transplant survival benefit model for individualized risk prediction of HCC and non-HCC related mortality with and without liver transplantation, allowing for differential prioritization of HCC candidates.
To cite this abstract in AMA style:
Tran BV, Lapisatepun W, Dumronggittigule W, Markovic D, Lee Y, Kaldas F, Farmer D, Busuttil R, Agopian V. A Intention-to-Treat Analysis of 881 Consecutively Waitlisted Patients to Develop a Survival Benefit Model for Hepatocellular Carcinoma Liver Transplant Candidates [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/a-intention-to-treat-analysis-of-881-consecutively-waitlisted-patients-to-develop-a-survival-benefit-model-for-hepatocellular-carcinoma-liver-transplant-candidates/. Accessed July 12, 2025.« Back to 2022 American Transplant Congress