Implications of Subclinical Borderline Acute Cellular Rejection Detected in Protocol Biopsies on Graft Outcomes.
1Glickman Urological and Kidney institute, Cleveland Clinic, Cleveland, OH
2Internal Medicine, Univ. Hospitals Case Medical Center, Cleveland, OH.
Meeting: 2016 American Transplant Congress
Abstract number: 138
Keywords: Biopsy, Graft function, Kidney transplantation, Rejection
Session Information
Session Name: Concurrent Session: Kidney Immune Monitoring 1
Session Type: Concurrent Session
Date: Sunday, June 12, 2016
Session Time: 4:30pm-6:00pm
 Presentation Time: 5:42pm-5:54pm
Presentation Time: 5:42pm-5:54pm
Location: Ballroom C
Background: The effects of subclinical borderline acute cellular rejection (BACR-defined as I1T1 per Banff criteria) detected in protocol biopsies (Bx) on subsequent graft function and histology are unknown. Moreover, whether the treatment of this pathological finding is beneficial to the graft is also debatable.
Methods: We studied 212 renal transplant recipients who underwent (3-6, 12 & 24 mos) protocol Bx. Patients were divided into 3 cohorts based on the initial biopsy findings: 1) normal; 2) BACR treated with steroids; and 3) BACR not treated with steroids. Outcome were graft function (eGFR) and any Bx proven rejection for the 3 cohorts at subsequent Bx, either for cause or protocol.
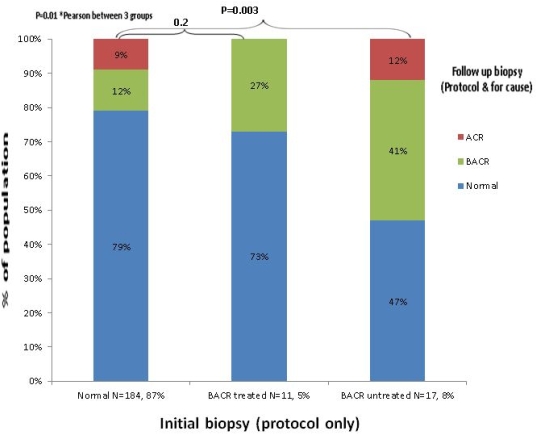
Results: Mean age±SD was 49±13 yo, 39.6% were female and 21.2% were AA. BACR was diagnosed in 13% of the patients. There was no statistical significant demographic differences b/w groups, nor there was difference in terms of ESRD cause, donor type, cold/warm ischemia times, immunosuppressive therapy, DGF and follow up duration. Median nbr of days (10th-90thPCT) from transplant to first Bx was 121 (90-221). At 24 mos post transplant, recipients with initial protocol Bx reported as normal or treated BACR had statistically significant lower incidence of BACR and new ACR (Banff 1A or greater) (21% and 27% respectively) compared to those with non-treated BACR, 53%, p=0.003) (see figure). There was a trend to higher eGFR in the first two groups compared to those with non-treated BACR patients (57±19, 52±19 and 47±29 ml/min/1.73m2, respectively).
Conclusions: Our data suggest a higher incidence of ACR and/or persistence of subclinical BACR in subsequent Bx of patients where BACR is diagnosed on protocol Bx and is not treated. This finding might also be associated with a lower eGFR in those with BACR who receive no treatment. Further studies are needed to demonstrate the negative impact of subclinical BACR found in protocol Bx on graft histology and function, and benefits of treatment with steroids.
CITATION INFORMATION: Zaky Z, Yu C, Elfadawy N, Chiesa-Vottero A, Herlitz L, Flechner S, Poggio E. Implications of Subclinical Borderline Acute Cellular Rejection Detected in Protocol Biopsies on Graft Outcomes. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Zaky Z, Yu C, Elfadawy N, Chiesa-Vottero A, Herlitz L, Flechner S, Poggio E. Implications of Subclinical Borderline Acute Cellular Rejection Detected in Protocol Biopsies on Graft Outcomes. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/implications-of-subclinical-borderline-acute-cellular-rejection-detected-in-protocol-biopsies-on-graft-outcomes/. Accessed January 27, 2026.« Back to 2016 American Transplant Congress
