Anti-IL6R Therapy (Tocilizumab) Improves Long-Term Patient & Graft Survival in Patients with Chronic Antibody-Mediated Rejection and Transplant Glomerulopathy.
Comprehensive Transplantation Center, Cedars-Sinai Medical Center, Los Angeles, CA.
Meeting: 2016 American Transplant Congress
Abstract number: 416
Keywords: Graft survival, Highly-sensitized, HLA antibodies, Kidney transplantation
Session Information
Session Name: Concurrent Session: Kidney Immunosuppression: Novel Agents
Session Type: Concurrent Session
Date: Tuesday, June 14, 2016
Session Time: 2:30pm-4:00pm
 Presentation Time: 3:18pm-3:30pm
Presentation Time: 3:18pm-3:30pm
Location: Veterans Auditorium
Introduction:Extending the functionality of renal allografts is an essential goal of transplant medicine. HS patients (pts) are at increased risk for chronic ABMR (CABMR) due to immunodominant donor specific antibodies (iDSAs).There are limited options for prevention and treatment (Rx) of CABMR & TG. Pts who develop TG post-tx have a dismal prognosis. Here we report on our extended experience with TCZ for Rx for CABMR & TG. Patients & Methods: From 4/2011 we identified 34 CABMR+ pts including those with chronic TG and iDSA+. 5/34 (14.7%) were pediatric (age range 7-18). Pts received TCZ at 4-8mg/kg monthly for 3-15 doses and f/u to 24M. Pts were monitored for iDSA relative intensity scores (RIS; 0 = No DSA; 2 = <5000MFI(weak); 5= 5000-104MFI (moderate);10= >104MFI (strong), renal function, & pt/graft survival. Results: The mean time from tx to TCZ Rx was 6±4.3Y. 30/34(88%) pts had significant pathologic findings of ABMR and TG. The majority of iDSAs were class II (DQs, 25/30(83%). After Rx, reductions in mean iDSA RIS were seen (7.3±3.3 at 0M vs 4.8±4.0 at 12M, p=0.02). Mean GFRs (42.2±17.8ml/min at 0M vs. 46.3±18.2ml/min at 18M) stabilized through Rx. Four pts had repeat biopsies >1Y after initiation of TCZ. 3/4 had clear improvement in Banff scores with elimination of C4d+ staining. Outcomes for a separate cohort of HS patients (n=41) with CABMR & TG treated with IVIG + Rituximab +/- PLEX (SOC) were compared with TCZ treated pts (n=34). 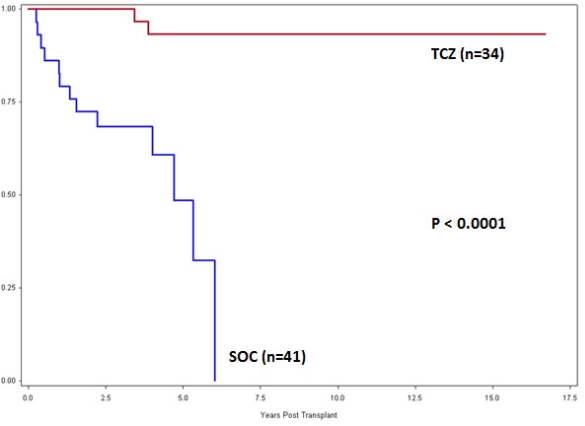 Data shows a significant improvement in long-term graft survival for the TCZ group. In addition, pts in the SOC who lost their grafts had higher death rates (p=0.002). Conclusions: CABMR & TG pts treated with TCZ continue to show long term stabilization of renal function and improved survivals. Although there is a benefit in reduction of iDSAs, there may be other beneficial mechanisms of action of anti-IL6-R therapy. More importantly, extending the functional half-life of allografts has benefits for the patient in improving length and quality of life and to the health care system.
Data shows a significant improvement in long-term graft survival for the TCZ group. In addition, pts in the SOC who lost their grafts had higher death rates (p=0.002). Conclusions: CABMR & TG pts treated with TCZ continue to show long term stabilization of renal function and improved survivals. Although there is a benefit in reduction of iDSAs, there may be other beneficial mechanisms of action of anti-IL6-R therapy. More importantly, extending the functional half-life of allografts has benefits for the patient in improving length and quality of life and to the health care system.
CITATION INFORMATION: Choi J, Vo A, Haas M, Puliyanda D, Louie S, Peng A, Kahwaji J, Villicana R, Kim I, Mirocha J, Jordan S. Anti-IL6R Therapy (Tocilizumab) Improves Long-Term Patient & Graft Survival in Patients with Chronic Antibody-Mediated Rejection and Transplant Glomerulopathy. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Choi J, Vo A, Haas M, Puliyanda D, Louie S, Peng A, Kahwaji J, Villicana R, Kim I, Mirocha J, Jordan S. Anti-IL6R Therapy (Tocilizumab) Improves Long-Term Patient & Graft Survival in Patients with Chronic Antibody-Mediated Rejection and Transplant Glomerulopathy. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/anti-il6r-therapy-tocilizumab-improves-long-term-patient-graft-survival-in-patients-with-chronic-antibody-mediated-rejection-and-transplant-glomerulopathy/. Accessed February 27, 2026.« Back to 2016 American Transplant Congress
