Outcomes of Highly-Sensitized, Virtual and Flow Cross-Match Negative Renal Transplant Recipients: A Retrospective Observational Study
1Transplant Nephrology, Mayo Clinic, Rochester, MN, 2Laboratory Medicine and Pathology, Mayo Clinic, Rochester, MN
Meeting: 2022 American Transplant Congress
Abstract number: 1413
Keywords: Antibodies, HLA antibodies, Rejection, Sensitization
Topic: Clinical Science » Kidney » 45 - Kidney Chronic Antibody Mediated Rejection
Session Information
Session Name: Kidney Chronic Antibody Mediated Rejection
Session Type: Poster Abstract
Date: Monday, June 6, 2022
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: Many highly-sensitized kidney transplant recipients are sensitized from prior transplants, which have been shown to limit graft survival more than pregnancy or blood transfusions. Non-HLA donor-specific antibodies (DSAs) may play a role, though their long-term effects have never been examined in this population. Characterizing graft outcomes of highly-sensitized, cross-match negative recipients can elucidate the effect of non-HLA DSAs on allograft survival.
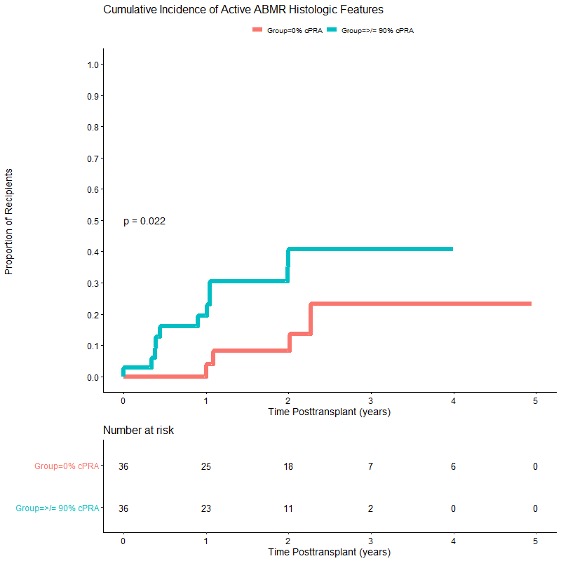
*Methods: We performed a single-center, retrospective, matched cohort study comparing outcomes of kidney transplant recipients with cPRA >/= 90% (n=36) and cPRA = 0% (n=36). Patients were matched by age and donor type. Those with pretransplant DSA and de novo DSA (defined as MFI>1000) were excluded, after reviewing LABSCREEN single antigen bead testing and flow cytometric results with our HLA laboratory. Surveillance biopsies and de novo DSA screening were performed 4, 12, 24 and 60 months post-transplant. We used Banff 2019 criteria (except for DSA) for the histologic diagnosis of ABMR. Non-HLA antibodies were not tested for.
*Results: Baseline characteristics were similar among the matched cohorts. The median (IQR) age was 46.0 (34.7, 55.4); 80.6% were Caucasian, and 62.5% received a deceased donor kidney transplant. 52.8% of patients with cPRA>/= 90% were female, compared to 33.3% in the cPRA = 0% cohort (p=0.10). Despite having no pretransplant DSA, recipients with a cPRA >/= 90% had a higher incidence of histologic features suggestive of active antibody-mediated rejection (ABMR) (30.6% (11/36) versus 11.1% (4/36), p=0.04) over a median (IQR) follow-up time of 3.2 (2.2, 3.9) years post-transplant. Glomerulitis and peritubular capillaritis were the predominant histologic features of ABMR. While no patient with cPRA >/= 90% and histologic features of ABMR developed de novo DSA, all patients with active ABMR in the cPRA = 0% group developed de novo DSA. Death-censored allograft survival was lower among patients with a cPRA >/= 90% (88.9% versus 97.2%), though not statistically significant (p=0.16).
*Conclusions: Highly-sensitized transplant recipients have a higher incidence of histologic features of ABMR, even in the absence of anti-HLA DSA. Non-HLA DSAs may play a larger role than previously accredited, though further work is needed to characterize their mechanisms of injury and impact on long-term allograft survival.
To cite this abstract in AMA style:
Agrawal A, Smith B, Gandhi M, Schinstock C. Outcomes of Highly-Sensitized, Virtual and Flow Cross-Match Negative Renal Transplant Recipients: A Retrospective Observational Study [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/outcomes-of-highly-sensitized-virtual-and-flow-cross-match-negative-renal-transplant-recipients-a-retrospective-observational-study/. Accessed February 14, 2026.« Back to 2022 American Transplant Congress