End-to-Side Splenic to Hepatic Artery Reconstruction in Liver Transplant: A Case Series
Department of Surgery, University of Utah School of Medicine, Salt Lake City, UT
Meeting: 2022 American Transplant Congress
Abstract number: 1439
Keywords: Hepatic artery, Liver, Liver grafts, Liver transplantation
Topic: Clinical Science » Liver » 57 - Liver: Surgery Innovative Techniques*
Session Information
Session Name: Liver: Surgery Innovative Techniques*
Session Type: Poster Abstract
Date: Monday, June 6, 2022
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: Optimal hepatic artery (HA) blood flow post-liver transplantation (LT) is necessary for long-term allograft success. HA thrombosis (HAT) contributes to significant morbidity and mortality after LT. An aortic jump graft (infrarenal and supraceliac) is most commonly considered to optimize HA inflow in instances where the native HA is not adequate. We present a case series where the native splenic artery is used for HA reconstructed in an end-to-side anastomosis.
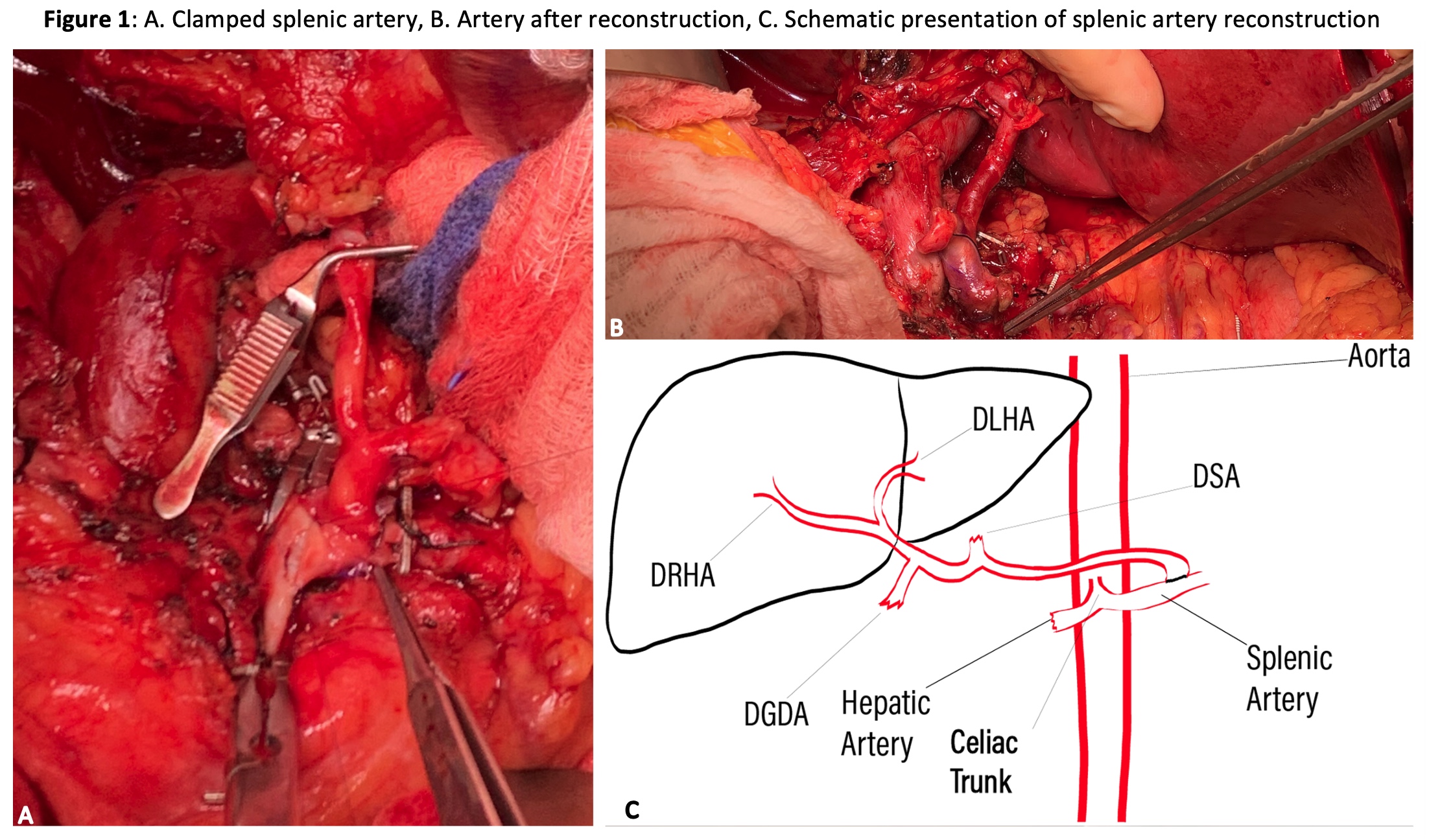
*Methods: In this case series, we report five liver transplantation cases where the native splenic artery was used for HA reconstruction. Standard LT was performed using a piggyback technique for caval reconstruction and end to end for portal vein. The common hepatic artery (CHA) was found to be unfit for reconstruction. Three cases were redo liver transplants, and in two cases intimal dissection of CHA was noted during hepatectomy. The splenic artery (SA) was then exposed and dissected free of its surrounding tissue. A clamp is placed in a side-biting fashion on the SA, an arteriotomy was performed, and an aortic punch expands the arteriotomy. The celiac trunk of the graft was anastomosed using a 6-0 Prolene. An end-to-side anastomosis using the donor celiac axis is fashioned to the arteriotomy of the SA. The donor splenic and left gastric arteries were ligated. The LT then proceeded in the standard fashion.
*Results: Doppler US on all patients was performed on day 1 and 3 postop as per institutional protocol. Excellent arterial waveforms were demonstrated. One PT required post-transplant splenectomy for significant splenic steal. One patient also required hepatic artery dilation without the need for stenting about 16 weeks following the transplant.
*Conclusions: This report presents a novel approach to HA reconstruction using an end-to-side anastomosis to the SA. The SA often has more than adequate length and diameter, allowing a tension free anastomosis with adequate flow for the liver graft. In conclusion, we present an acceptable technique for extra-anatomic HA reconstruction using SA inflow.
| Patient #1 | Patient #2 | Patient #3 | Patient #4 | Patient #5 | |
| Case Type | Redo Liver Tx | Intimal dissection | Redo Liver Tx | Redo Liver Tx |
Intimal dissection |
| Age | 58 | 32 | 42 | 61 | 35 |
| BMI | 32.39 | 23.56 | 22.04 | 34.56 | 27.04 |
| Tx Indication | ESLD | ESLD | EoTH | ESLD second to NASH/EoTH | ESLD second to EoTH |
| Diabetes | No | T1 | No | T2 | T2 |
To cite this abstract in AMA style:
Baker N, Aviles-Ovalle L, Baker T, Campsen J, Kim R, Rofaiel G. End-to-Side Splenic to Hepatic Artery Reconstruction in Liver Transplant: A Case Series [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/end-to-side-splenic-to-hepatic-artery-reconstruction-in-liver-transplant-a-case-series/. Accessed January 15, 2026.« Back to 2022 American Transplant Congress