Impact of Arterial Reconstruction Technique on Hepatic Arterial Thrombosis in a Decade of Pediatric Liver Transplantation
1Surgery, University of Cincinnati College of Medicine, Cincinnati, OH, 2Surgery, Cincinnati Children's Hospital Medical Center, Cincinnati, OH
Meeting: 2022 American Transplant Congress
Abstract number: 1445
Keywords: Graft failure, Hepatic artery, Liver transplantation, Pediatric
Topic: Clinical Science » Liver » 61 - Liver: Pediatrics
Session Information
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
Session Information
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Hall C
*Purpose: Hepatic artery thrombosis (HAT) is a morbid and potentially fatal complication following pediatric liver transplantation (PLT). Previous registry studies have identified preoperative characteristics associated with HAT; however, they have been unable to directly evaluate the impact of arterial reconstruction techniques on HAT incidence.
*Methods: All PLTs performed between 2010-2020 at a single institution were included. Preoperative and intraoperative characteristics, allograft type, and anastomotic reconstruction techniques were evaluated for their association with HAT.
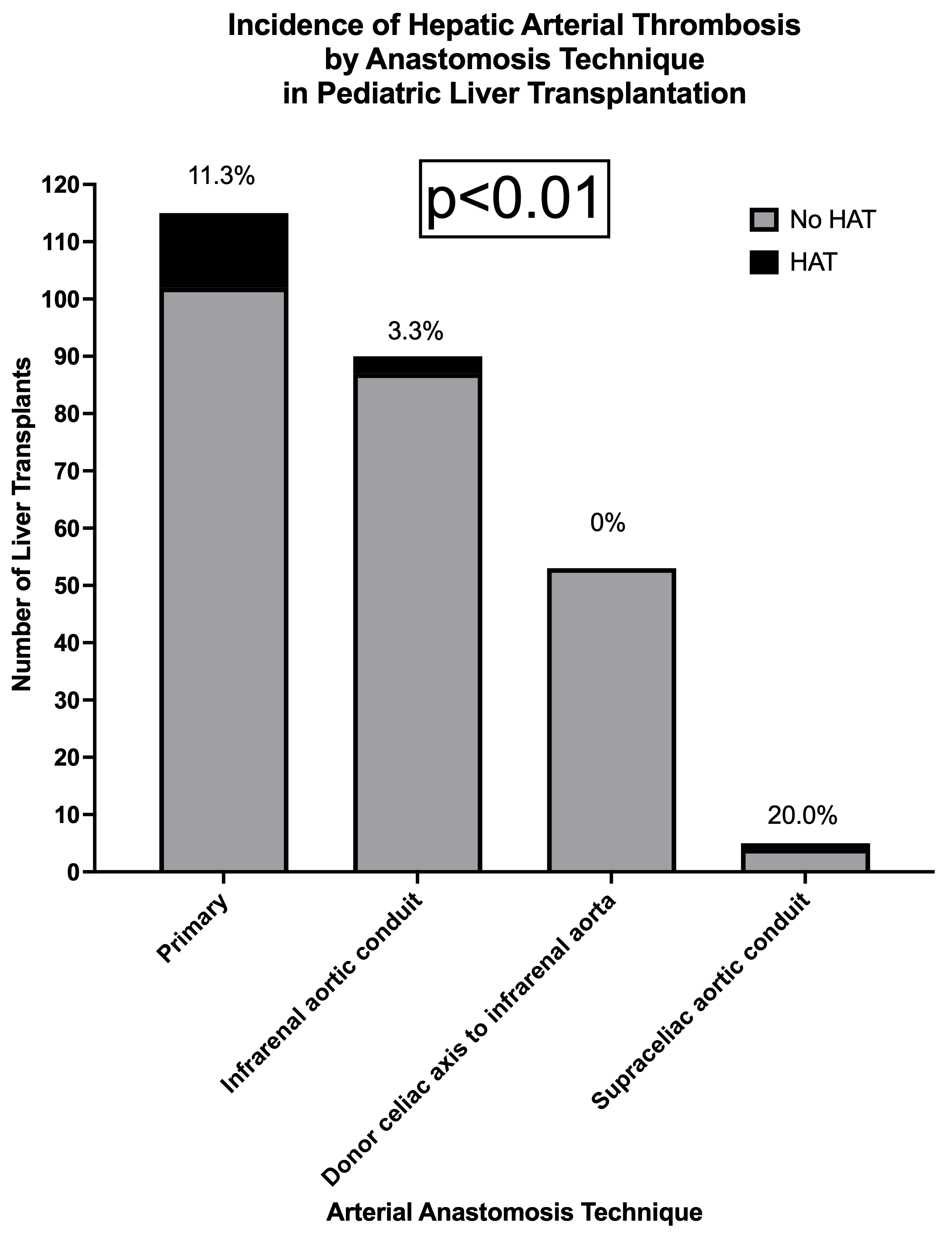
*Results: 263 consecutive patients underwent PLT. 115 (43.7%) underwent primary arterial anastomosis, 90 (34.2%) had an infrarenal aortic conduit placed, 53 (20.2%) had the donor celiac axis anastomosed to the infrarenal aorta (end-to-side), and 5 (1.9%) underwent placement of a supraceliac aortic conduit. 17 (6.5%) recipients had HAT requiring intervention. HAT was significantly decreased in recipients who had the donor celiac axis anastomosed to the infrarenal aorta, followed by infrarenal aortic conduit, primary anastomosis, and then supraceliac aortic conduit (0% vs 3.3% vs 11.3% vs 20%, p<0.01, FIGURE 1). Furthermore, after adjusting for type of allograft and recipient age, an end-to-side anastomosis from the celiac axis to the infrarenal aorta or placement of an infrarenal aortic conduit remained associated with decreased HAT incidence when compared to a primary anastomosis (p=0.02, TABLE 1).
*Conclusions: When technically feasible, creating an end-to-side infrarenal aortic anastomosis utilizing the donor celiac axis or an infra-renal aortic conduit can protect against HAT when compared to primary anastomosis in PLT.
| Clinical characteristic | Univariable OR [95% CI] | p-Value | Multivariable OR [95% CI] | p-Value |
| Recipient age | 1.07 [1.00-1.15] | 0.05 | 0.99 [0.91-1.08] | 0.78 |
| Technical variant graft vs. whole | 0.35 [0.11-1.09] | 0.05 | 0.43 [0.12-1.59] | 0.19 |
| Arterial reconstruction technique | <0.01 | 0.02 | ||
| Primary | Ref | Ref | ||
| Infrarenal aortic conduit | 0.27 [0.07-0.98] | 0.04 | 0.23 [0.06-0.96] | 0.04 |
| Donor celiac axis to infrarenal aorta | < 0.01 | – | < 0.01 | – |
| Supraceliac aortic conduit | 1.96 [0.20-18.91] | 0.56 | 1.59 [0.47-99.71] | 0.16 |
To cite this abstract in AMA style:
Delman AM, Farooqi Z, Schepers E, Bondoc A, Tiao G, Mullapudi B. Impact of Arterial Reconstruction Technique on Hepatic Arterial Thrombosis in a Decade of Pediatric Liver Transplantation [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/impact-of-arterial-reconstruction-technique-on-hepatic-arterial-thrombosis-in-a-decade-of-pediatric-liver-transplantation/. Accessed January 23, 2026.« Back to 2022 American Transplant Congress