Liver Transplantation for Combined Hepatocellular-Cholangiocarcinoma: An Analysis of the European Liver Transplant Registry
1HPB and Transplant Surgery, Erasmus MC, Rotterdam, Netherlands, 2Multi-Organ Transplant Program, University Health Network, Toronto, ON, Canada
Meeting: 2022 American Transplant Congress
Abstract number: 1104
Keywords: Hepatocellular carcinoma, Liver transplantation, Malignancy, Surgery
Topic: Clinical Science » Liver » 56 - Liver: Hepatocellular Carcinoma and Other Malignancies
Session Information
Session Name: Liver: Hepatocellular Carcinoma and Other Malignancies
Session Type: Poster Abstract
Date: Sunday, June 5, 2022
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: Little is known about combined hepatocellular-cholangiocarcinoma (cHCC-CCA) demographics and their long-term outcomes after liver transplantation (LT). By analysing data from the European Liver Transplant Registry (ELTR), we aimed to map cHCC-CCA character traits and identify patient subgroups that demonstrate favourable long-term outcomes after the receipt of a LT for cHCC-CCA.
*Methods: ELTR-centers with cHCC-CCA patients transplanted between 1985-2021 were identified and contacted for study participation. Overall survival (OS) and recurrence-free survival (RFS) curves were estimated using the Kaplan-Meier test and compared by log-rank. To assess true recurrence, a cumulative incidence approach was used, considering death without recurrence as a competing event.
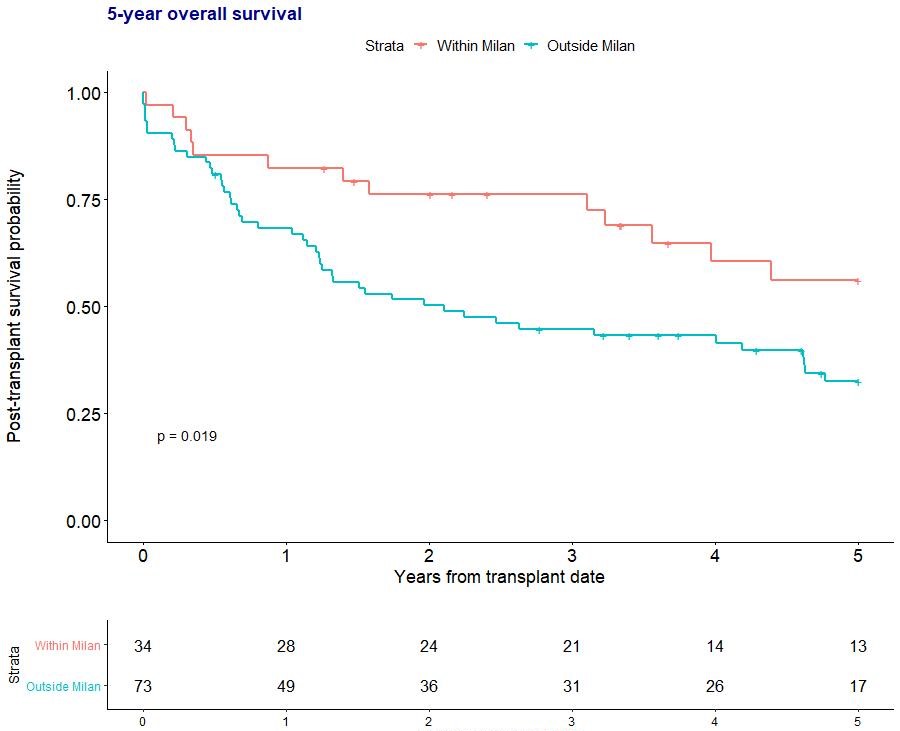
*Results: A total of 115 transplanted cHCC-CCA patients from 22 different centers were analyzed. The majority were male (83%). Seventy-nine (69%) patients were listed as HCC, while only 4 were diagnosed with cHCC-CCA pre-operatively (3%). Most common underlying diseases were alcoholic liver disease (35%), hepatitis C virus (25%), and hepatitis B virus (17%). Median tumour number at listing was 2 (IQR 2-2), with a median maximum size of 28mm (IQR 20-41mm). Tumour markers pre-LT were on median: AFP 15 (IQR 5-67), CA19.9 26 (IQR 13-58), CEA 3.3 (2.0-5.3). Before LT, 56% received TACE, 17% liver resection, and 15 % RFA. Explant pathology showed a median tumour number of 2 (IQR 1-4), maximum size of 32mm (23-50mm), with vascular invasion present in 40%. OS at 1, 3, 5-years was 70%, 51%, 37%, where RFS was 60%, 40%, 32%. Cumulative incidence of recurrence was 22%, 39%, and 42% at 1, 3 and 5-years. Within vs. outside Milan at listing showed an OS of 72%, 62%, 45% vs. 71%, 34%, 24% at 1, 3, and 5-years (p = 0.03), where a similar distinction pre-LT showed OS rates of 77%, 65%, 49% vs. 62%, 33%, 23% (p < 0.01). Explant pathology separated survival rates in 82%, 76%, 56% within Milan vs. 68%, 45%, 32% outside Milan at 1, 3, and 5 years (p = 0.02), where RFS was 82%, 62%, 54% within Milan and 53%, 33%, 25% outside Milan (p < 0.01). Based on size and number, no subgroups demonstrated superior survival.
*Conclusions: Most cHCC-CCA patients were male and diagnosed post-LT after being listed for HCC. Alcoholic liver disease was the most common underlying liver disease. OS for patients within Milan yielded acceptable 5-years rates, superior to those outside Milan. Nonetheless, recurrence rates were generally high.
To cite this abstract in AMA style:
Claasen MP, Ivanics T, IJzermans JN, Sapisochin G, Polak W. Liver Transplantation for Combined Hepatocellular-Cholangiocarcinoma: An Analysis of the European Liver Transplant Registry [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/liver-transplantation-for-combined-hepatocellular-cholangiocarcinoma-an-analysis-of-the-european-liver-transplant-registry/. Accessed February 21, 2026.« Back to 2022 American Transplant Congress