Fontan versus Non-Fontan Combined Heart-Liver Transplantation: Proceed but Cautiously
Vanderbilt University Medical Center, Nashville, TN
Meeting: 2022 American Transplant Congress
Abstract number: 1127
Keywords: Heart transplant patients, Heart/lung transplantation, Liver transplantation, Survival
Topic: Clinical Science » Heart » 63 - Heart and VADs: All Topics
Session Information
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
Session Information
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Hall C
*Purpose: Combined heart-liver transplantation (CHLT) is increasing, corresponding with a growing prevalence of Fontan-associated end-organ damage. We aimed to describe our contemporary institutional experience with CHLT and compare our Fontan and non-Fontan CHLT recipients.
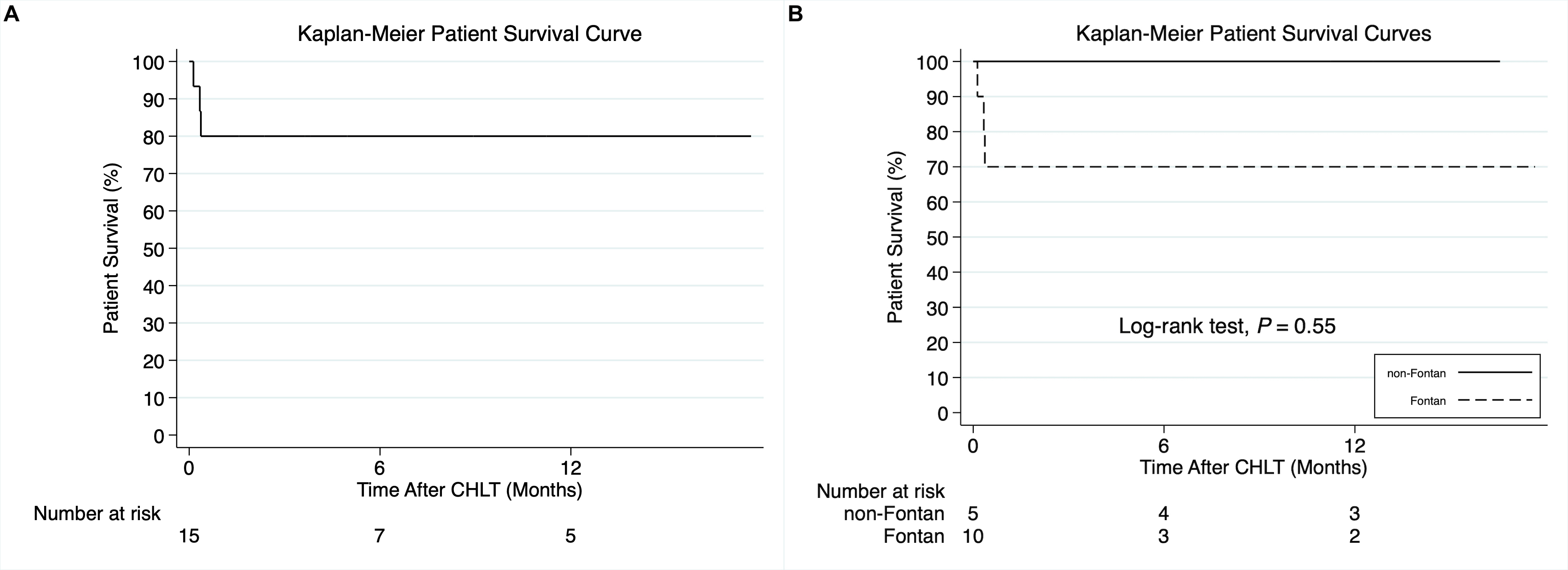
*Methods: All consecutive CHLTs performed at a single high-volume transplant center between April 2017 and November 2021 were included. Patient characteristics were described with summary statistics and survival analysis was performed using the Kaplan-Meier method and the log-rank test.
*Results: 15 consecutive adult recipients underwent sequential CHLT. Cardiac indication was Fontan failure (10), Shone syndrome (1), ischemic cardiomyopathy (1), non-ischemic cardiomyopathy (1), Adriamycin cardiomyopathy (1), and hemochromatosis (1). Liver indication was Fontan-associated liver disease (10), cardiac cirrhosis (2), HCV cirrhosis (2), and hemochromatosis (1). The median age at CHLT was 38 years (interquartile range [IQR]: 34-51), 73.3% were men, and the median waitlist time was 27 days (IQR: 15-104). The median MELD-XI score was 12.6 (IQR: 9.4-15.4) and the median VAST (varices, ascites, splenomegaly, thrombocytopenia) score was 2 (IQR: 2-3). Compared to non-Fontan recipients, Fontan recipients were younger (median 36 vs 50 years, p=0.051) but had longer cardiopulmonary bypass (median 199 vs 126 minutes, p=0.01) and operative times (median 817.5 vs 599 minutes, p=0.01), and larger yet not statistically significant blood product transfusion requirements (median 12.8L vs 6.3L, p=0.25). Five of 15 patients required perioperative extracorporeal membrane oxygenation (ECMO). Of the five, 3 were Fontan patients who subsequently died. Six patients (40%) underwent unplanned re-operation including chest exploration (3), abdominal exploration (1), and combined chest and abdominal exploration (2). The 1-year overall patient survival was 80% (Figure A). The 1-year patient survival was 70% for Fontan and 100% for non-Fontan CHLT recipients (p=0.55; Figure B).
*Conclusions: Although feasible, CHLT for the treatment of Fontan associated end-organ disease is particularly challenging and associated with higher recipient morbidity compared to non-Fontan related CHLT. Advances in cardioprotective strategies during the liver transplant portion of CHLT in Fontan recipients may improve outcomes in this growing high-risk population.
To cite this abstract in AMA style:
Ziogas IA, Wu WK, Izzy M, Shingina A, Benson C, Mishra KL, Shah AS, Do NL, McMaster WG, Menachem JN, Alexopoulos SP. Fontan versus Non-Fontan Combined Heart-Liver Transplantation: Proceed but Cautiously [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/fontan-versus-non-fontan-combined-heart-liver-transplantation-proceed-but-cautiously/. Accessed February 16, 2026.« Back to 2022 American Transplant Congress