Pulsatile Kidney Perfusion Improves Survival and Graft Function in High Acuity Combined Liver Kidney Transplant (CLKT) Recipients
1Surgery, Rutgers New Jersey Medical School, Newark, NJ, 2Division of Transplant and Hepatobiliary Surgery, Rutgers New Jersey Medical School, Newark, NJ, 3Rutgers State University of New Jersey, Montclair, NJ, 4Rutgers New Jersey Medical School, Morris Plains, NJ, 5Surgery/ Transplant, Rutgers New Jersey Medical School, Newark, NJ, 6Rutgers New Jersey Medical School, Newark, NJ
Meeting: 2022 American Transplant Congress
Abstract number: 1080
Keywords: Ischemia, Kidney/liver transplantation, Machine preservation, Pulsatile preservation
Topic: Clinical Science » Liver » 52 - Liver: Kidney Issues in Liver Transplantation
Session Information
Session Name: Liver: Kidney Issues in Liver Transplantation
Session Type: Poster Abstract
Date: Sunday, June 5, 2022
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: Due to underlying renal dysfunction, CLKT recipients tend to have higher medical acuity at baseline resulting in a higher likelihood of post-operative complications and graft dysfunction. The role of pulsatile kidney perfusion in this setting is not yet clearly defined. The purpose of the present study was to evaluate all patients receiving CLKT in the US and to analyze the subgroups that might benefit most from pre-transplant kidney machine perfusion.
*Methods: The OPTN database was queried for all adult CLKT recipients between 2003-2017. Patients were stratified by MELD and kidney cold ischemia time (kCIT). Recipient survival and delayed graft function (DGF) was compared in patients receiving pumped (pCLKT) versus non-pumped (nCLKT) kidneys.
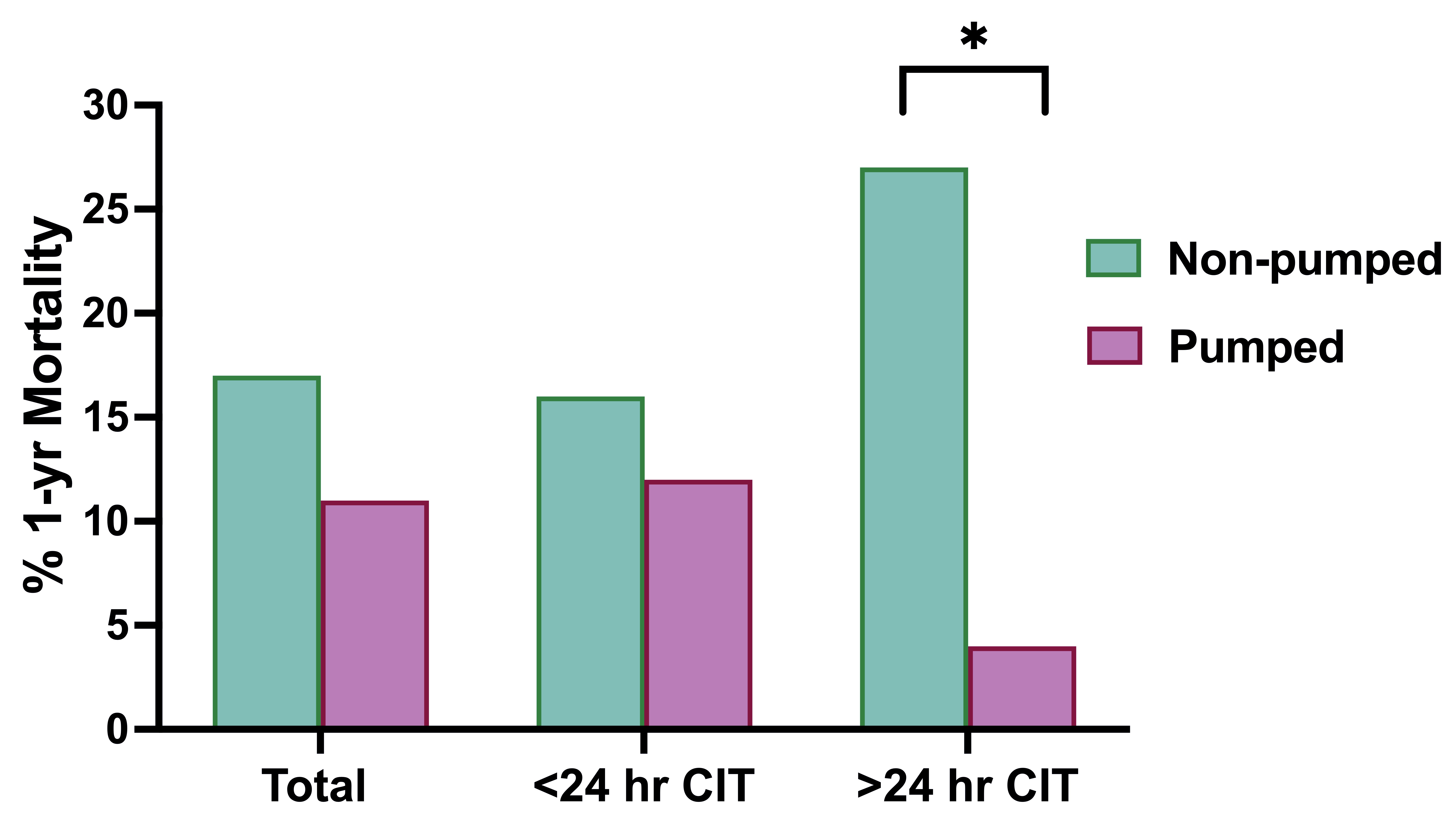
*Results: 4214 CLKT recipients were identified, 24% pCLKT and 76% nCLKT. Median biologic MELD, donor, and recipient characteristics were similar between groups. Patient survival was similar between groups, with 1- and 5-year mortality of 12.4% and 43.7% for pCLKT, and 14.8% and 40.1% for nCLKT (p=0.07); however, there was a significantly decreased incidence of DGF in pCLKT (18% pCLKT vs 24% nCLKT, p=0.002). This difference was especially remarkable with kCIT >24 hrs (23% vs 49%, p=0.0001). Subgroup analysis of recipients with >24hrs kCIT receiving pCKLT revealed a trend for decreased 1-yr mortality and improved rates of DGF across all MELD scores. Amongst recipients with highest acuity (MELD>35), pCLKT resulted in markedly improved 1-yr mortality (5% pCLKT vs 22% nCLKT, p=0.03) and decreased DGF (33% vs. 54%, p<0.05), Figure 1.
*Conclusions: The benefit of kidney machine perfusion in CLKT has been the subject of much debate, and is not routinely employed. These data suggest that a subgroup of patients may greatly benefit from this modality. In the setting of prolonged kidney cold ischemia (eg hemodynamic instability or bleeding following liver implant) and in patients with high medical acuity at the time of transplant (ie high MELD), we observe a substantial benefit in kidney allograft function and overall patient mortality incurred by perioperative pumping of the kidney prior to CLKT.
To cite this abstract in AMA style:
Liu T, Panayotova G, Paterno F, Amin A, Brown L, Guarrera J, Lunsford K. Pulsatile Kidney Perfusion Improves Survival and Graft Function in High Acuity Combined Liver Kidney Transplant (CLKT) Recipients [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/pulsatile-kidney-perfusion-improves-survival-and-graft-function-in-high-acuity-combined-liver-kidney-transplant-clkt-recipients/. Accessed March 1, 2026.« Back to 2022 American Transplant Congress