Ex Vivo Liver Resection and Autotransplantation – Should It Be Used More Frequently?
1Columbia University Irving Medical Center, New York, NY, 2University of Iowa, Iowa City, IA, 3Atrium Health, Charlotte, NC, 4University of Florida, Gainesville, FL
Meeting: 2022 American Transplant Congress
Abstract number: 131
Keywords: Hepatocellular carcinoma, Liver, Malignancy, Split-liver transplantation
Topic: Clinical Science » Liver » 57 - Liver: Surgery Innovative Techniques*
Session Information
Session Name: Surgery innovative Techniques Including Living Donor
Session Type: Rapid Fire Oral Abstract
Date: Sunday, June 5, 2022
Session Time: 5:30pm-7:00pm
 Presentation Time: 5:30pm-5:40pm
Presentation Time: 5:30pm-5:40pm
Location: Hynes Room 313
*Purpose: Ex vivo liver resection expands the limits of resectability for advanced liver tumors but remains underutilized due to concerns about technical complexity and vascular thrombosis. We herein present the largest collective American ex vivo experience to evaluate long-term outcomes and perioperative morbidity.
*Methods: We retrospectively analyzed 35 cases performed by surgical teams experienced with ex vivo liver resections (at least 4 cases) between 1997-2021.
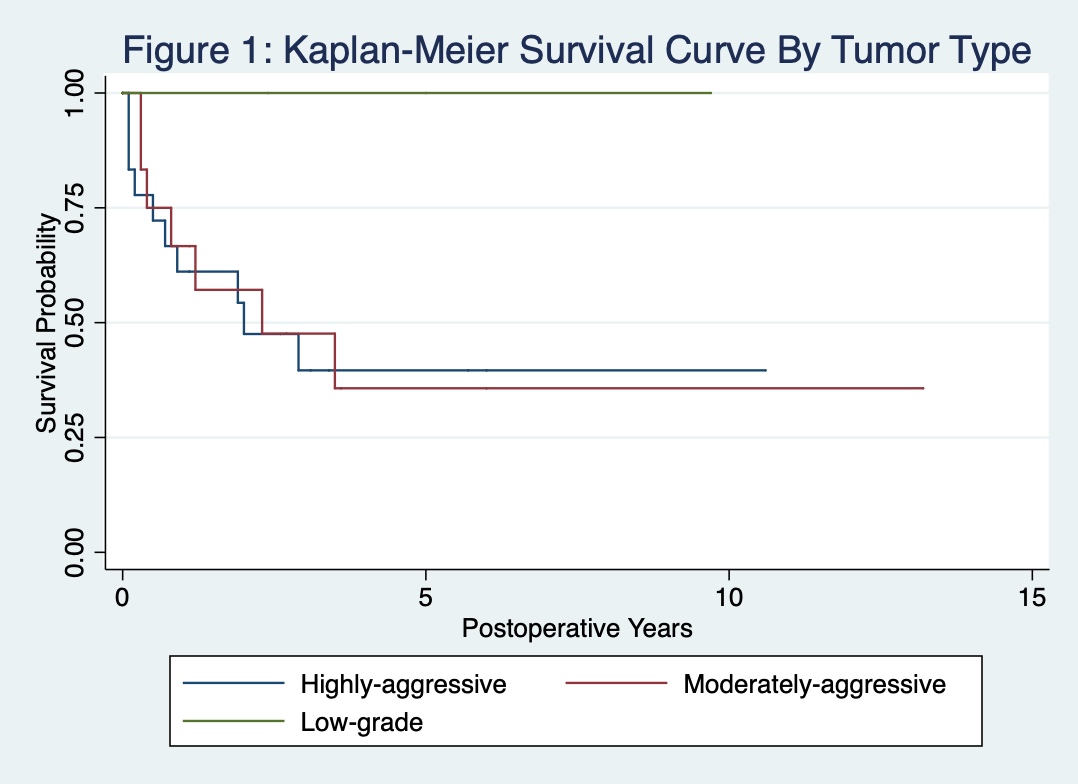
*Results: We categorized tumors as highly-aggressive (n = 18), moderately-aggressive (n = 14), and less-aggressive (n =3). Highly-aggressive tumors included cholangiocarcinoma (n = 10) and sarcoma (n = 8); moderately-aggressive tumors included colorectal metastastes (n = 8), fibrolamellar hepatocellular carcinoma (n = 4), and hepatocellular carcinoma (n = 2); less-aggressive tumors included biliary cystadenocarcinoma, neuroblastoma, and primary neuroendocrine tumor (each n = 1). One additionally required right nephrectomy and two required adrenalectomy. Eighteen of 35 patients (51%) are currently alive with a median follow up of 3.14 years. The overall survival was 67.7%/49.2%/44.1%, at 1-/3-/5-years, respectively (Figure 1). Patient survival for highly-aggressive, moderately-aggressive, and less aggressive tumors was 61.1%/40.2%/40.3%, 69.2%/49.1%/35.1%, and 100%/100%/100% at 1-/3-/5-years, respectively (Figure 2). We achieved R0 resection in 30/35 (85.7%) patients. Seventeen (48.6%) tumors recurred in a mean of 353 days (range 25-1239). 30-day mortality was limited to one case (2.9%). Two additional patients (5.8%) died between 30 and 90 days. There was no vascular thrombosis.
*Conclusions: Ex vivo liver resection utilizes techniques commonly practiced in partial liver transplantation and provides the opportunity for tumor resection and vascular reconstruction with less warm ischemic time, improved exposure, less time pressure, and less bleeding. Our data, representing the largest series of ex vivo hepatic resections to date, demonstrate reasonable long-term survival rates with low perioperative morbidity and vascular complications as well as the ability to achieve R0 margins in otherwise unresectable tumors. We propose that more liberal use of this technique may benefit selected patients in centers experienced with partial liver transplantation.
To cite this abstract in AMA style:
Weiner J, Griesemer A, Hemming A, Levi D, Beduschi T, Matsumoto R, Mathur A, Emond J, Kato T. Ex Vivo Liver Resection and Autotransplantation – Should It Be Used More Frequently? [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/ex-vivo-liver-resection-and-autotransplantation-should-it-be-used-more-frequently/. Accessed March 5, 2026.« Back to 2022 American Transplant Congress