First Report of Xenotransplantation from a Pig to Human Recipient
1NYU Langone Transplant Institute, New York, NY, 2CUMC, New York, NY
Meeting: 2022 American Transplant Congress
Abstract number: 81
Keywords: Hyperacute rejection, Kidney transplantation, knockout, Xenoreactive antibodies
Topic: Basic Science » Basic Science » 13 - Xenotransplantation
Session Information
Session Time: 3:30pm-5:00pm
 Presentation Time: 4:10pm-4:20pm
Presentation Time: 4:10pm-4:20pm
Location: Hynes Room 302
*Purpose: Xenotransplantation of genetically edited pig organs into human recipients can solve the global scarcity of organs for transplantation. Humans lack the α1,3-Gal glycan ubiquitously expressed on pig cells. Naturally occurring anti-α1,3-Gal antibodies can cause hyperacute rejection of porcine xenografts. We report the first instance of xenotransplantation of a kidney from an α1,3-Gal knock-out (KO) pig to a recently deceased human.
*Methods: We performed two successful xenotransplants in 2021. Both recipients were brain-dead organ and research donors but were found to have organs unsuitable for transplantation. Under a protocol approved by the NYU institutional committee for research on the deceased, the decedents’ families authorized whole body donation for a study of xenotransplantation. Kidneys from α1,3-Gal KO pigs that had undergone prior autotransplantation of a thymic lobe were procured and transported to an isolation facility. The xenografts were implanted on the decedents’ femoral vessels for ease of observation, serial biopsies, and isolation of urine output from the native kidneys. Core biopsies were performed at 6, 12, 24, 36, and 48 hours. Immunosuppression consisted of methylprednisolone and mycophenolate mofetil until the kidneys were explanted at 54 hours.
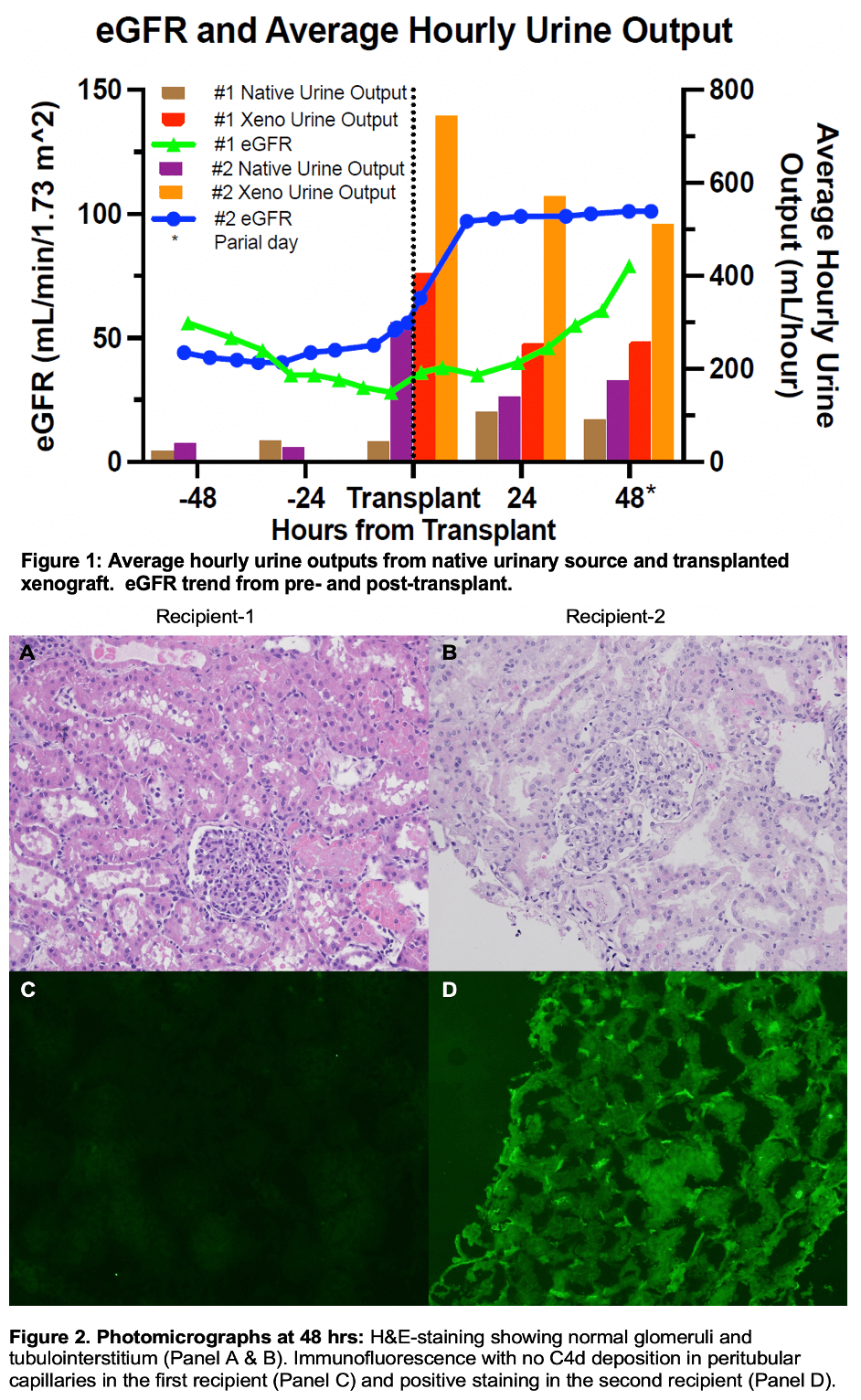
*Results: The xenografts immediately appeared pink and well-perfused and began to make urine. The cold ischemic times were 7 and 6 hours, respectively. In both cases, the decedents’ creatinine improved after implantation of the xenograft (Figure 1). The 48 hour post-reperfusion biopsy showed no evidence of AMR (Figure 2). Light microscopy revealed no interstitial inflammation, tubulitis, glomerular or peritubular microvascular inflammation. Significantly, immunohistochemical staining showed no C4d deposition in the peritubular capillaries in case 1. In case 2, there was C4d deposition but without the H&E features of AMR. Electron microscopy showed normal podocyte morphology. Core biopsies at 12, 24, and 36 hours showed similar findings.
*Conclusions: Our study serves as proof of concept that α1,3-Gal KO organs can be transplanted into humans without the risk of accelerated AMR and that xenotransplantation was associated with improved creatinine. Our study also supports similar data from porcine-to-primate xenotransplant studies and paves the way for human clinical trials.
To cite this abstract in AMA style:
Stern J, Tatapudi V, Lonze B, Stewart Z, Mangiola M, Wu M, Mehta S, Weldon E, Dieter R, Lawson N, Griesemer A, Parent B, Piper G, Sommer P, Cawthon S, Sullivan B, Ali N, Montgomery RA. First Report of Xenotransplantation from a Pig to Human Recipient [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/first-report-of-xenotransplantation-from-a-pig-to-human-recipient/. Accessed February 21, 2026.« Back to 2022 American Transplant Congress