Characterizing the Landscape of Cancer Risk Following HLA-Incompatible Living Donor Kidney Transplantation
1Johns Hopkins University, Baltimore, MD, 2National Cancer Institute, Bethesda, MD, 3University of Wisconsin-Madison, Madison, WI
Meeting: 2022 American Transplant Congress
Abstract number: 65
Keywords: Highly-sensitized, HLA antibodies, Kidney, Malignancy
Topic: Clinical Science » Organ Inclusive » 67 - Non-PTLD/Malignancies
Session Information
Session Name: PTLD and Malignancies
Session Type: Rapid Fire Oral Abstract
Date: Sunday, June 5, 2022
Session Time: 3:30pm-5:00pm
 Presentation Time: 4:30pm-4:40pm
Presentation Time: 4:30pm-4:40pm
Location: Hynes Room 309
*Purpose: Incompatible living donor kidney transplant recipients (ILDKTr) require desensitization to facilitate transplantation across donor-specific antibody (DSA); however, this substantial upfront immunosuppression may result in serious complications, including cancer.
*Methods: We compared 858 ILDKTr to 12,239 compatible LDKT recipients (CLDKTr) drawn from a US multicenter cohort with novel linkage to the Transplant Cancer Match Study from 1997-2016. We characterized DSA strength as positive-Luminex, negative-flow crossmatch (PLNF); positive-flow, negative-cytotoxic crossmatch (PFNC); or positive-cytotoxic crossmatch (PCC). We characterized the landscape of cancer risk in ILDKTr using propensity score weighted Cox regression models, and corrected for multiple comparisons using the false discovery rate.
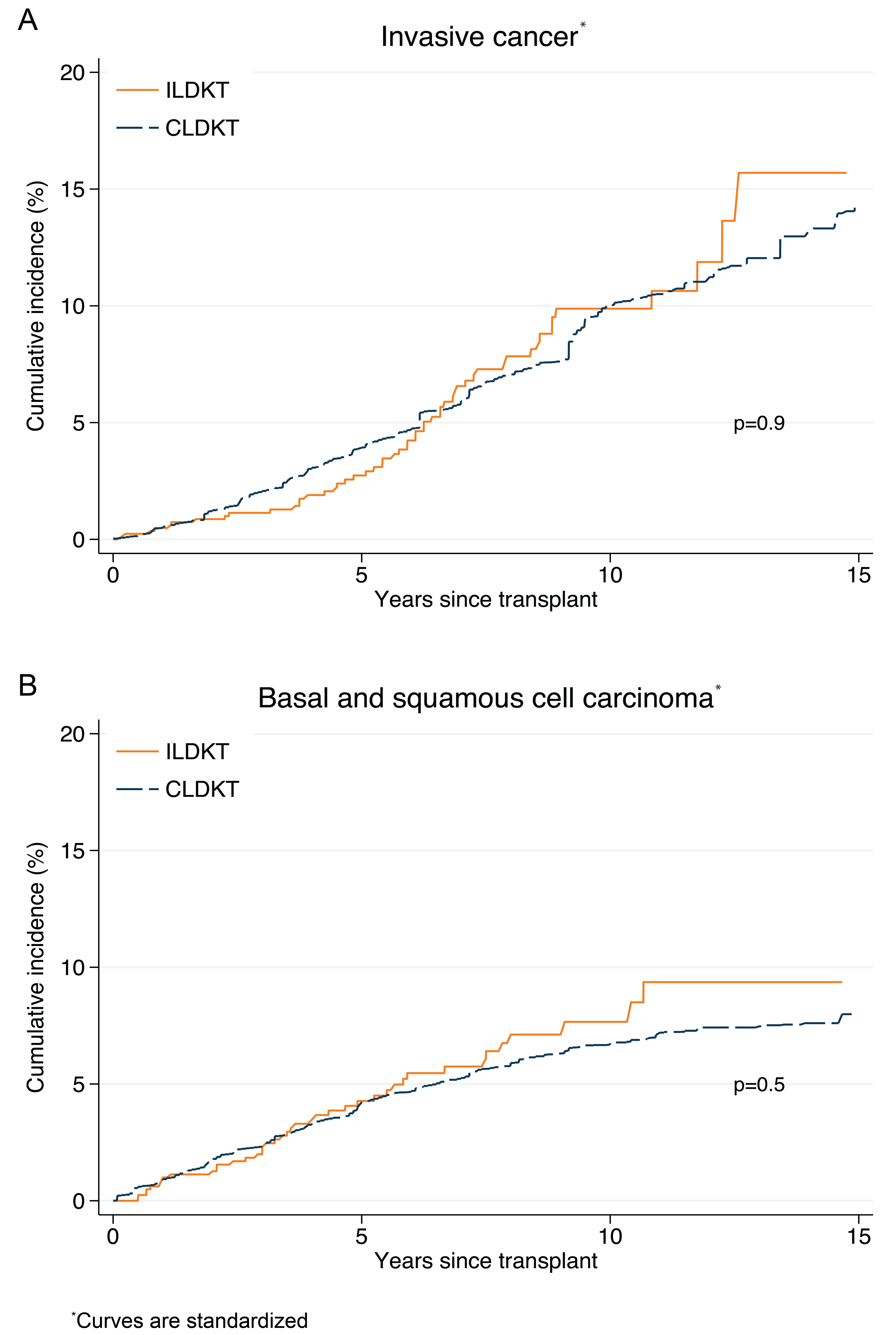
*Results: Invasive cancers occurred in 811 of CLDKT, 9 of PLNF, 28 of PFNC, 16 of PCC recipients, which did not translate into a statistically significant difference for ILDKTr (weighted hazard ratio [wHR]: PLNF=0.530.971.77;PFNC=0.681.061.65;PCC=0.590.991.65 vs. CLDKT; 15-year absolute risk, ILDKT: 15.7% vs. CLDKT: 14.2%) (Figure 1A). Similar trends persisted across most cancer sites. Although ILDKTr had higher risk of gastrointestinal cancers compared to CLDKTr (wHR=1.032.305.13, p=0.04), this difference was not significant after correction for multiple comparisons. Basal and squamous cell carcinomas of the skin occurred in 737 of CLDKT, 6 of PLNF, 24 of PFNC, 11 of PCC recipients (wHR PLNF=0.440.851.63;PFNC=0.681.222.21; PCC=0.591.152.25 vs. CLDKT; 15-year absolute risk, ILDKT: 9.4% vs. CLDKT: 8.0%) (Figure 1B).
*Conclusions: In this multicenter study, there was no evidence of increased cancer risk associated with ILDKT. While careful monitoring is warranted, these findings support the use of ILDKT for recipients when compatible living donors are not available.
To cite this abstract in AMA style:
Motter JD, Jackson K, Yu K, Pfeiffer RM, Massie A, Garonzik-Wang J, Segev D, Engels EA. Characterizing the Landscape of Cancer Risk Following HLA-Incompatible Living Donor Kidney Transplantation [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/characterizing-the-landscape-of-cancer-risk-following-hla-incompatible-living-donor-kidney-transplantation/. Accessed February 12, 2026.« Back to 2022 American Transplant Congress