Alloimmunization Against Red Blood Cell Antigens is Not Associated with Increased All Cause Mortality in Liver Transplant Recipients
1Department of Pathology, Northwestern University Feinberg School of Medicine, Chicago, IL, 2Department of Surgery, Northwestern University Feinberg School of Medicine, Chicago, IL
Meeting: 2022 American Transplant Congress
Abstract number: 882
Keywords: Alloantibodies, Alloantigens, Liver, Survival
Topic: Clinical Science » Liver » 55 - Liver: Recipient Selection
Session Information
Session Time: 5:30pm-7:00pm
 Presentation Time: 5:30pm-7:00pm
Presentation Time: 5:30pm-7:00pm
Location: Hynes Halls C & D
*Purpose: Liver transplantation (LT) is a life‐saving procedure for patients with end‐stage liver disease and transfusion therapy of LT patients remains a challenge. Improvement of LT outcomes requires better understanding of factors leading to reduced survival. Some evidence suggests that red blood cell alloantibodies (RBCA) are associated with reduced survival. A retrospective study evaluating transfusion records and all cause mortality (ACM) between 2002-2021 in LT recipients was completed. To our best knowledge this is the largest cohort of RBCA analyzed in LT recipients.
*Methods: Adult LT and transfusion records were reviewed (2002-2021). Patients undergoing repeat transplantation or combined transplantation of liver with other organs were excluded.
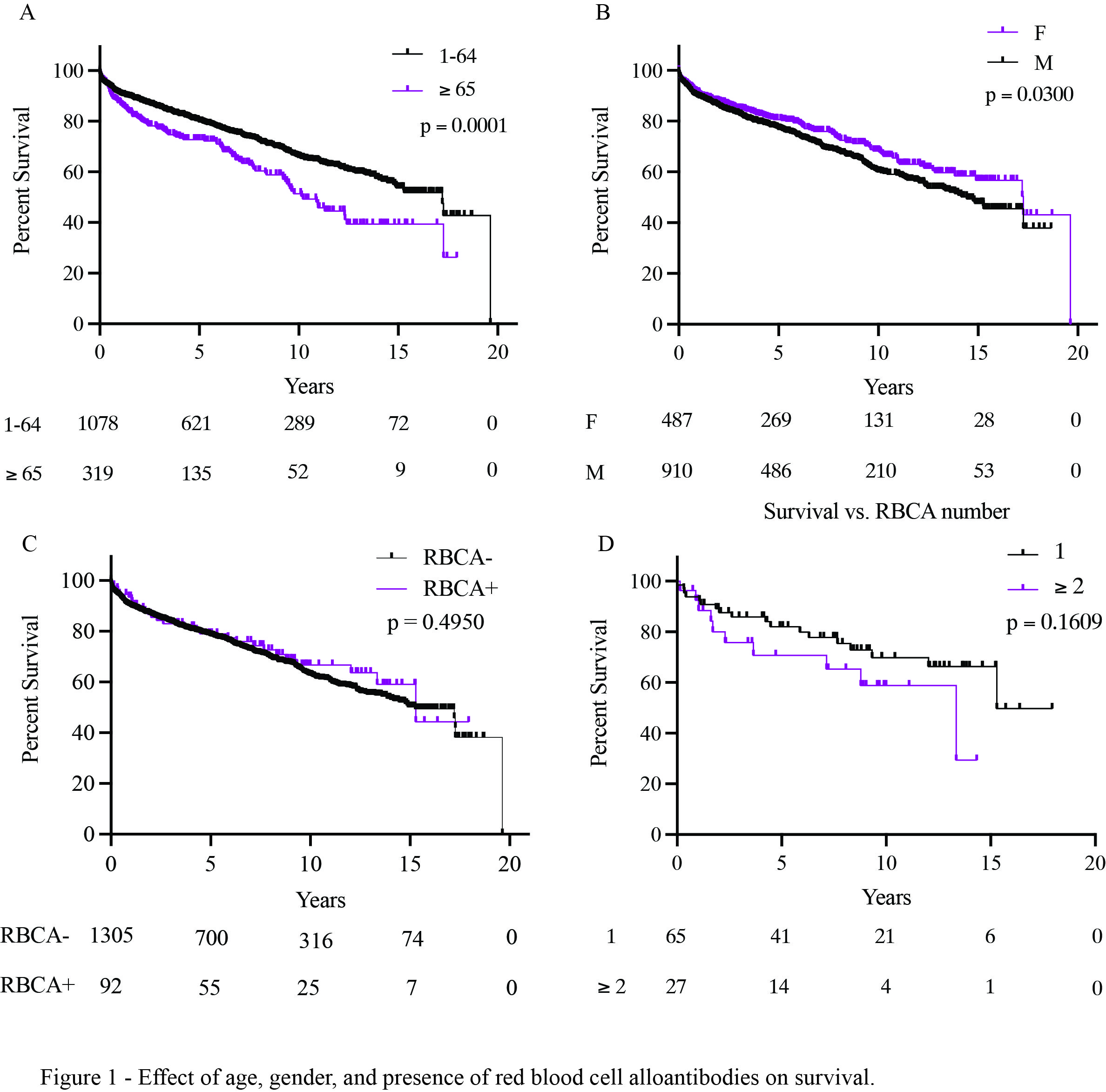
*Results: Between 2002-2021, 2079 LTs were completed, 1397 met inclusion criteria (1305 RBCA-, 92 RBCA+). The RBCA- and RBCA+ cohorts did not differ in age (55.83 (17-79) vs. 56.80 (25-72), p=0.4114, respectively), or gender (RBCA-, M 859 (65%), F 446 (35%) vs. RBCA+, M 51 (55%); F 41 (45%), p = 0.0538). Total of 153 RBCA were detected, the 10 most common were: E (39.13%), Jka (22.82%), K (18.47%), C (11.95%), M (8.69%), D (7.60%), Fya (6.52%), e (4.43%), c (3.26), Jkb (3.26). Twenty-seven patients (29.34%) contained >1 RBCA. The common groups were: C, Jka (7.40)% and E, Dia (7.40%). ACM was increased in males (males, 14.45 years median survival (yms) vs. female; 17.26 yms, p = 0.030) and patients ≥65 y (≥65 10.2 yms vs <64 17.21 yms, p<0.0001). Presence of RBCA (one or more) did not affect ACM (RBCA- 15.26 yms vs. RBCA+ 15.29 yms, p = 0.4950). The top 5 most common causes of death in the RBCA- group were infection, primary malignancy (solid), recurrent disease (malignant), cardiovascular arrest, and respiratory failure. The top 5 most frequent causes of death in RBCA+ group were recurrent disease (non-malignant), infection, recurrent disease (malignant), primary malignancy (solid), and cardiovascular (myocardial infarction).
*Conclusions: To our best knowledge this is the largest study evaluating ACM in LT patients with RBCA. Results suggest that the survival of RBCA+ LT recipients is no different than RBCA- LT recipients. These patients do not have poorer outcomes in contrast to previously reported studies. Additionally, younger and female recipients have better survival relative to older and male recipients, respectively.
To cite this abstract in AMA style:
Chornenkyy Y, Gama AP, Khurram N, Booth AL, Leventhal JR, Ramsey GE, Yang G. Alloimmunization Against Red Blood Cell Antigens is Not Associated with Increased All Cause Mortality in Liver Transplant Recipients [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/alloimmunization-against-red-blood-cell-antigens-is-not-associated-with-increased-all-cause-mortality-in-liver-transplant-recipients/. Accessed February 18, 2026.« Back to 2022 American Transplant Congress