Liver Transplant Outcomes Using Grafts with Early Allograft Dysfunction
S. Y. Ohara1, E. Macdonough2, G. Mahdi3, L. Egbert3, B. Lizaola-Mayo2, W. Hewitt4, A. Mathur4, A. Moss4, K. Reddy4, B. Aqel4, C. Jadlowiec4
1Division of Surgery, Valleywise Health Medical Center, Creighton University, Phoenix, AZ, 2Division of Gastroenterology and Hepatology, Mayo Clinic Arizona, Phoenix, AZ, 3Mayo Clinic Alix School of Medicine, Phoenix, AZ, 4Division of Transplant Surgery, Mayo Clinic Arizona, Phoenix, AZ
Meeting: 2022 American Transplant Congress
Abstract number: 889
Keywords: Donors, marginal, Donors, non-heart-beating, Graft survival, Liver transplantation
Topic: Clinical Science » Liver » 59 - Liver: Expanding the Donor Pool* (Liver: MELD Allocation / Donor Issues)
Session Information
Session Name: Liver: Expanding the Donor Pool* (Liver: MELD Allocation / Donor Issues)
Session Type: Poster Abstract
Date: Saturday, June 4, 2022
Session Time: 5:30pm-7:00pm
 Presentation Time: 5:30pm-7:00pm
Presentation Time: 5:30pm-7:00pm
Location: Hynes Halls C & D
*Purpose: The significance of early allograft dysfunction (EAD) and its impact on liver transplant (LT) outcomes remains debated. Our study aimed to assess LT outcomes specific to EAD and utilization of non-ideal donors.
*Methods: We assessed 611 LT at our center between 2015-2020 and compared outcomes between grafts with and without EAD. EAD was defined as bilirubin >10 mg/dL on day 7, INR >1.6 on day 7, or ALT and/or AST >2000 IU/L within the first 7 days of LT.
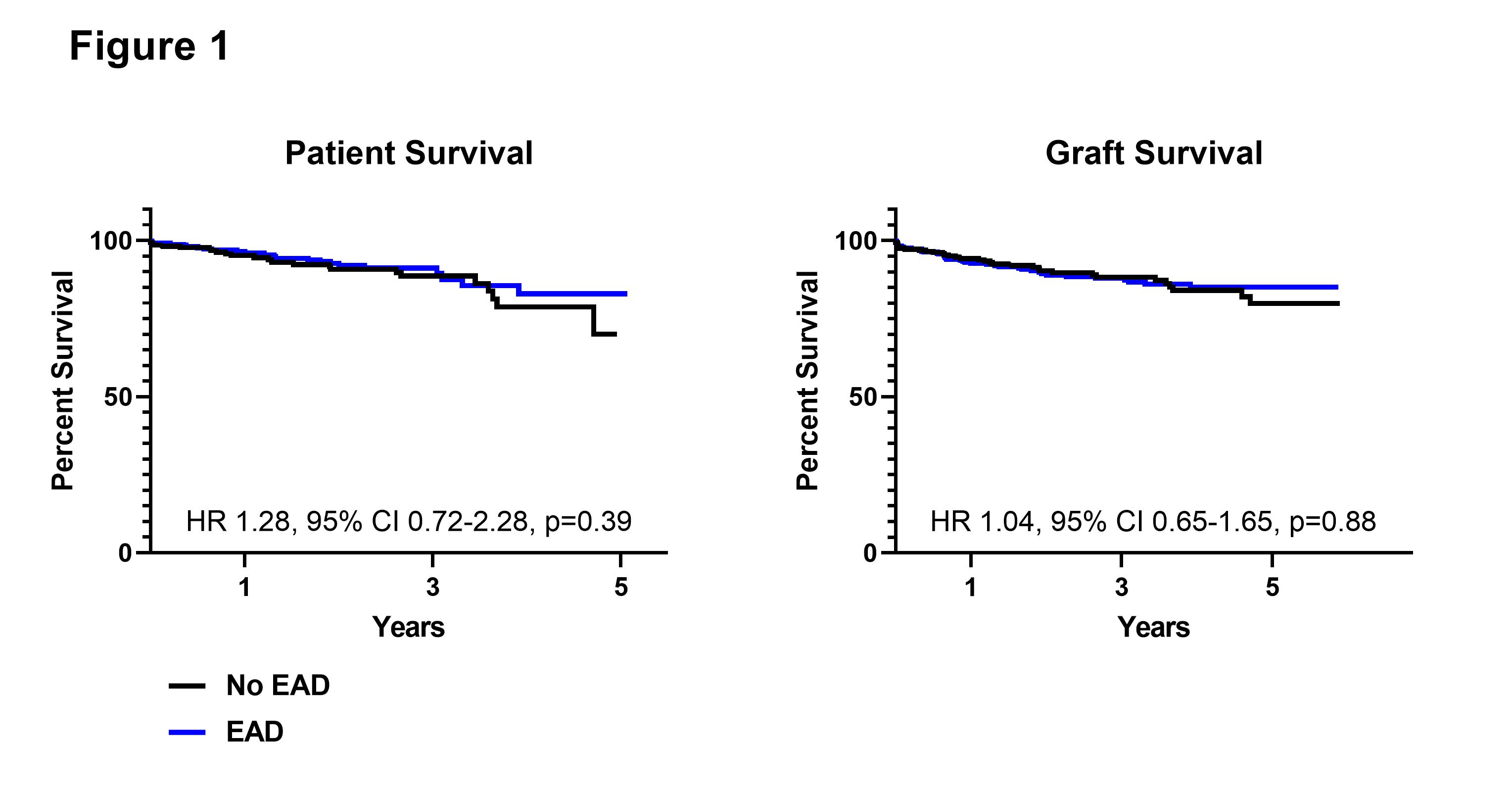
*Results: EAD was observed in 52.2% of LT. Grafts with EAD had higher donor risk index (DRI) scores (1.9 vs 1.6, p<0.0001). They were more likely to come from donation after circulatory death (DCD) donors (48% vs 13.8%, p<0.0001), be regionally allocated (p=0.003), and have higher cold ischemia times (6.0 vs 5.5 hours, p=0.001). EAD grafts were more likely to come from higher BMI donors (30.0 vs 26.8 kg/m2, p<0.0001) and have moderate steatosis (>30%) on biopsy (p<0.0001). Recipients of grafts with EAD had lower MELD scores (21 vs 23, p=0.0002) and were less likely to be re-transplants (p=0.003). The majority of grafts with EAD (89.1%) exhibited only 1 EAD criterion (AST>2000 in 1st week). Primary nonfunction events were rare (p=0.22) and there were no differences in ICU (2 vs 1 day, p=0.60) or hospital (6 vs 5 days, p=0.24) length of stay between EAD and non-EAD graft recipients. One-year patient survival for grafts with and without EAD was 96.9% and 94.1% (HR 1.28, 95% CI 0.72-2.28; p=0.39); 1-year graft survival was 93.1% and 92.1% (HR 1.04, 95% CI 0.65-1.65; p=0.88).
*Conclusions: With efforts to expand the donor pool, EAD occurrence has become more common. Post-transplant outcomes of non-ideal grafts with EAD can be similar to those of grafts without EAD in appropriately selected recipients. EAD is a predictable post-LT occurrence, particularly for DCD grafts, that can be managed expectantly, and should not be viewed as a deterrent to utilization.
| No EAD (n=290) | EAD (n=321) | P value | |
| Donor age (years) | 48.0±18.1 (50) | 48.5±13.0 (52) | 0.65 |
| Donor BMI (kg/m2) | 28.4±7.4 (26.8) | 31.0±8.3 (30.0) | <0.0001 |
| DRI | 1.6±0.5 (1.6) | 1.9±0.5 (1.9) | <0.0001 |
| Regional allocation | 137 (47.2%) | 198 (61.7%) | 0.0003 |
| DCD donor | 40 (13.8%) | 154 (48.0%) | <0.0001 |
| Graft with moderate steatosis | 11 (3.8%) | 42 (13.1%) | <0.0001 |
| CIT | 5.9±1.9 (5.5) | 6.4±1.9 (6.0) | 0.001 |
To cite this abstract in AMA style:
Ohara SY, Macdonough E, Mahdi G, Egbert L, Lizaola-Mayo B, Hewitt W, Mathur A, Moss A, Reddy K, Aqel B, Jadlowiec C. Liver Transplant Outcomes Using Grafts with Early Allograft Dysfunction [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/liver-transplant-outcomes-using-grafts-with-early-allograft-dysfunction/. Accessed February 27, 2026.« Back to 2022 American Transplant Congress