Incidence of Pancreatic Exocrine Insufficiency in Patients Undergoing Liver Transplantation
1Surgery, Rush University Medical Center, Chicago, IL, 2Surgery, Allegheny Health Network, Pittsburgh, PA, 3Hepatology, Rush University Medical Center, Chicago, IL
Meeting: 2021 American Transplant Congress
Abstract number: 648
Keywords: Liver cirrhosis, Liver transplantation, Post-operative complications
Topic: Clinical Science » Biomarkers, Immune Assessment and Clinical Outcomes
Session Information
Session Name: Biomarkers, Immune Assessment and Clinical Outcomes
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: The purpose of this study was to determine the incidence of Pancreatic Exocrine Insufficiency (PEI) in patients undergoing liver transplantation. Furthermore, patient-specific risk factors were identified, allowing for early recognition of PEI and treatment in order to improve malnutrition and post-transplant outcomes.
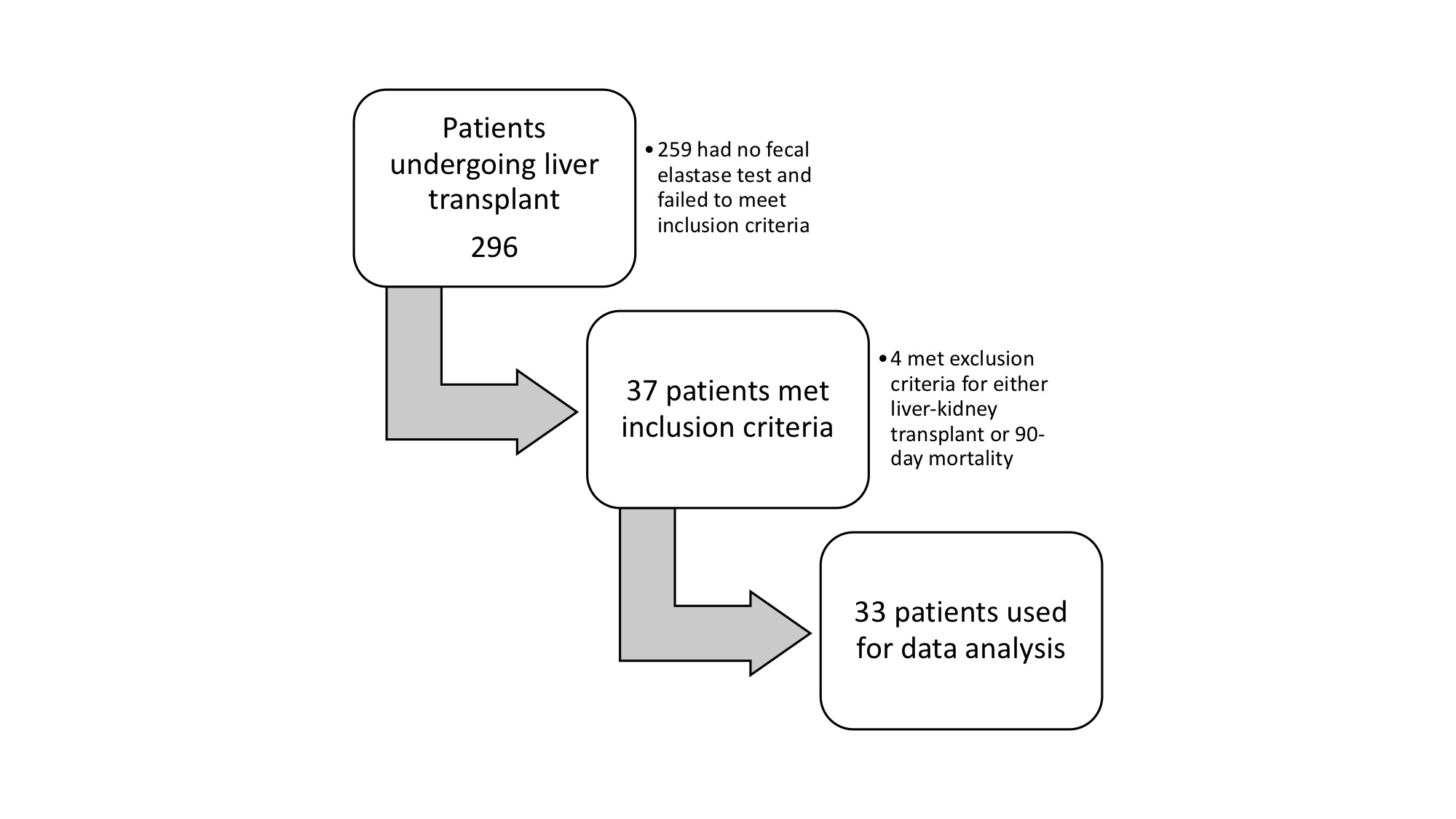
*Methods: A retrospective chart review of 296 consecutive patients undergoing liver transplantation at a single institution over 5 years was performed. After inclusion and exclusion criteria were applied, 33 patients were used for data analysis (Figure 1). Data collected included age, etiology, presence of diabetes, nutritional status prior to transplantation, and result of fecal elastase test. Survival data were compared to a control group (n=263) not receiving pancreatic enzymes.
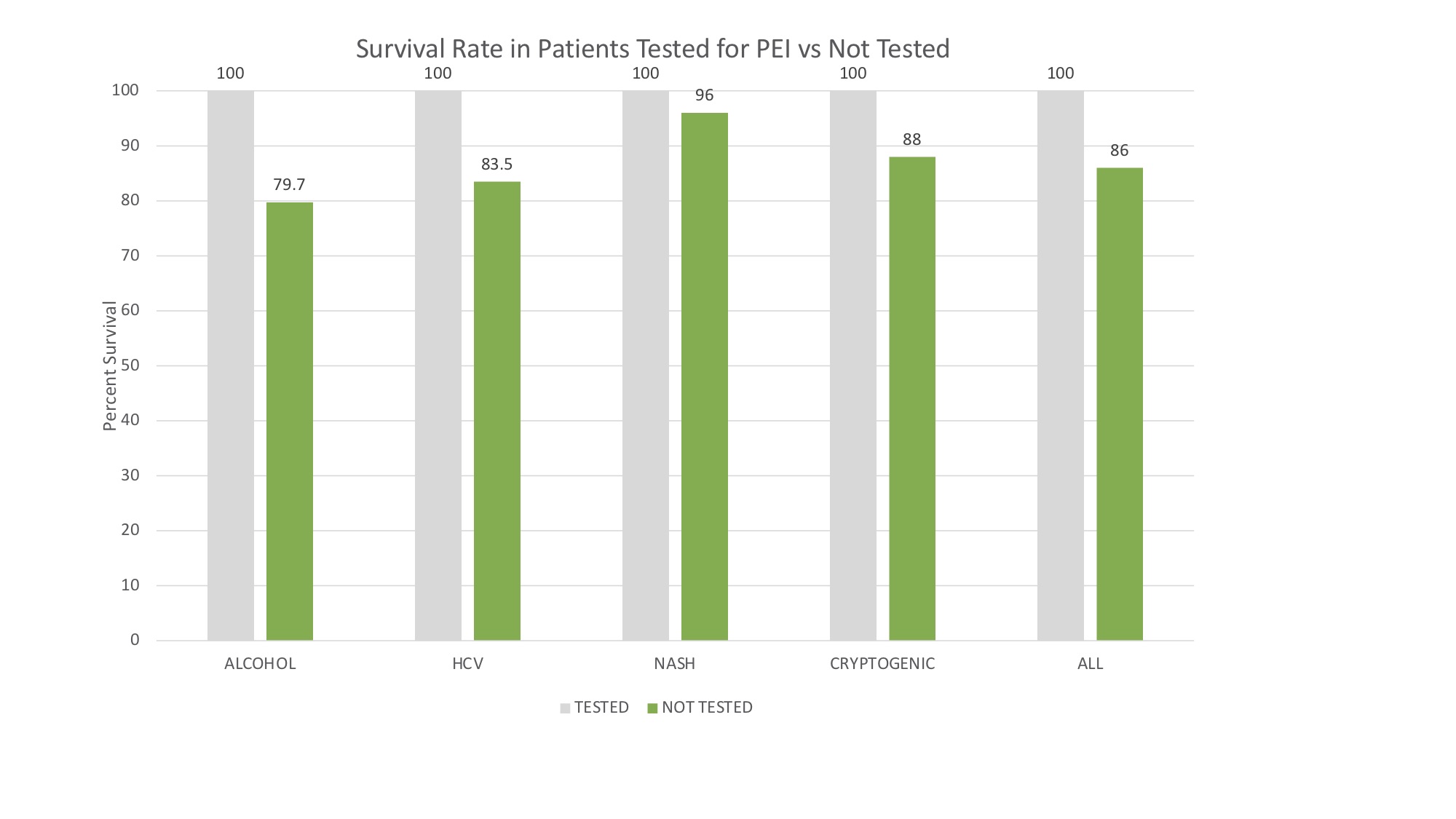
*Results: 33 charts were reviewed after having met inclusion criteria. The etiology of cirrhosis for transplant included NASH (5/33, 15.2%), alcoholic cirrhosis (17/33, 51.5%), hepatitis C (7/33, 21.2%) and cryptogenic (4/33, 12.1%). 18 patients (54.5%) were noted to have PEI, defined as fecal elastase <200 ug/g. There was a difference in rate of PEI (p=0.0059) when comparing different etiologies of cirrhosis. Rate of PEI in included patients with Hepatitis C (7/7, 100%) was highest, followed by cryptogenic (3/4, 75%), NASH (3/5, 60%) and alcohol (5/17, 29.4%). There was a significant difference in 1-year mortality among patients tested for PEI and those who weren't (p=0.009). For comparison by etiology see Figure 2.
*Conclusions: Symptomatic patients who were screened for PEI had a positivity rate of 54.5% (18/33). The cause of their cirrhosis played a significant role in the development of PEI, with Hepatitis C as the etiology most frequently associated with PEI and alcohol the least. Survival in general was significantly better for patients tested for PEI, suggesting a survival benefit of patient screening before transplantation. Further investigation into additional risk factors, as well as differences in outcomes with early supplementation, seems warranted.
To cite this abstract in AMA style:
Klein J, Rangel M, Ifearulundu I, Gely Y, Spigel Z, Janardhan S, Hertl M, Chan E. Incidence of Pancreatic Exocrine Insufficiency in Patients Undergoing Liver Transplantation [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/incidence-of-pancreatic-exocrine-insufficiency-in-patients-undergoing-liver-transplantation/. Accessed February 19, 2026.« Back to 2021 American Transplant Congress