Use of Granulocyte Colony Stimulating Factor After Lung Transplantation is Not Associated with Increased Likelihood of Acute Cellular Rejection
S. Fredrick1, C. Iasella2, L. Sacha3, R. Rivosecchi3, M. Morrell3, P. Sanchez3, J. Pilewski3, M. Snyder3, J. McDyer3, C. Moore3
1University of Rochester Medical Center, Rochester, NY, 2University of Pittsburgh School of Pharmacy, Pittsburgh, PA, 3University of Pittsburgh Medical Center, Pittsburgh, PA
Meeting: 2021 American Transplant Congress
Abstract number: 193
Keywords: Lung transplantation, Neutropenia, Rejection
Topic: Clinical Science » Lung » Lung: All Topics
Session Information
Session Name: When Opportunity Knocks... Identifying Interventions to Optimize Lung Transplant Outcomes
Session Type: Rapid Fire Oral Abstract
Date: Sunday, June 6, 2021
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:20pm-6:25pm
Presentation Time: 6:20pm-6:25pm
Location: Virtual
*Purpose: The cause of neutropenia in lung transplant recipients is multifactorial, including medications, viral infections, and antecedent disease. Granulocyte colony-stimulating factor (G-CSF) is commonly used to treat neutropenia in this population. This study examines whether the use of G-CSF is independently associated with acute cellular rejection (ACR) in lung transplant recipients.
*Methods: This was a matched cohort study of adult lung transplant recipients between January 2010 and October 2019. Patients who received G-CSF were matched 1:1 to those who did not based on transplant indication, age, and sex. The primary outcome was biopsy-proven ACR in the 6-month period after first G-CSF administration or from a matched post-transplant time point in the no G-CSF group. Variables with a p-value <0.2 were included with G-CSF in a multivariable logistic regression to assess their effect on likelihood of ACR. Secondary outcomes included time to first ACR, severity of ACR, chronic lung allograft dysfunction, survival, and infections.
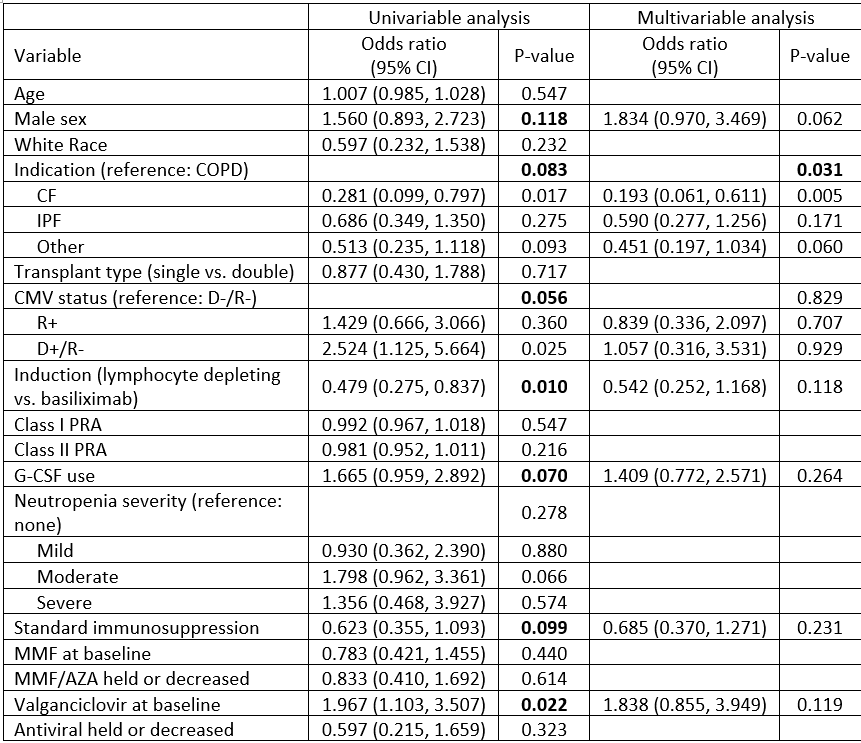
*Results: 212 patients were included in the final analysis (106 per group). Baseline characteristics were similar between groups, except there were more patients at high risk for cytomegalovirus (CMV) in the G-CSF group and more patients at low risk for CMV in the no G-CSF group. 50 (47.2%) patients in the G-CSF group experienced ACR in the first 6 months, compared to 37 (34.9%) in the no G-CSF group (p=0.070). Of those who experienced ACR, severity of ACR was similar between groups. Time to first rejection episode was shorter in the G-CSF group (p=0.049; figure 1). In a multivariable logistic regression analysis (table 1) with G-CSF use, male sex, transplant indication, CMV serostatus, type of induction, maintenance immunosuppression regimen, and use of valganciclovir/ganciclovir, use of G-CSF was not significantly associated with ACR at 6 months (OR (95% CI) 1.409 (0.772-2.571); p=0.264). Patients in the G-CSF group had a higher 1-year mortality rate and a higher incidence of EBV viremia and bacterial pneumonia. All other secondary outcomes were similar between groups.
*Conclusions: In this study in lung transplant recipients, G-CSF was not independently associated with ACR at 6 months. Treatment of neutropenia is often multimodal, and careful consideration of G-CSF therapy and other medication adjustments is warranted.
To cite this abstract in AMA style:
Fredrick S, Iasella C, Sacha L, Rivosecchi R, Morrell M, Sanchez P, Pilewski J, Snyder M, McDyer J, Moore C. Use of Granulocyte Colony Stimulating Factor After Lung Transplantation is Not Associated with Increased Likelihood of Acute Cellular Rejection [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/use-of-granulocyte-colony-stimulating-factor-after-lung-transplantation-is-not-associated-with-increased-likelihood-of-acute-cellular-rejection/. Accessed February 17, 2026.« Back to 2021 American Transplant Congress