Peripheral Blood Inflammatory Chemokines Uncover Rejection in the Absence of Histological Lesions
1Microbiology, Immunology and Transplantation, KU Leuven, Leuven, Belgium, 2Department of Transplantation, Nephrology and Clinical Immunology, Edouard Herriot Hospital Lyon, Lyon, France, 3Laboratory of Virology and Chemotherapy, KU Leuven, Leuven, Belgium
Meeting: 2021 American Transplant Congress
Abstract number: 396
Keywords: HLA antibodies, Inflammation, Kidney transplantation, Rejection
Topic: Clinical Science » Biomarkers, Immune Assessment and Clinical Outcomes
Session Information
Session Name: Biomarkers, Immune Assessment and Clinical Outcomes
Session Type: Poster Video Chat
Date: Saturday, June 5, 2021
Session Time: 7:30pm-8:30pm
 Presentation Time: 8:00pm-8:10pm
Presentation Time: 8:00pm-8:10pm
Location: Virtual
*Purpose: Cytokines and chemokines play a critical role in the pathophysiology of allograft rejection, but the relation of peripheral blood cytokine expression profiles to clinical kidney transplant rejection is insufficiently investigated.
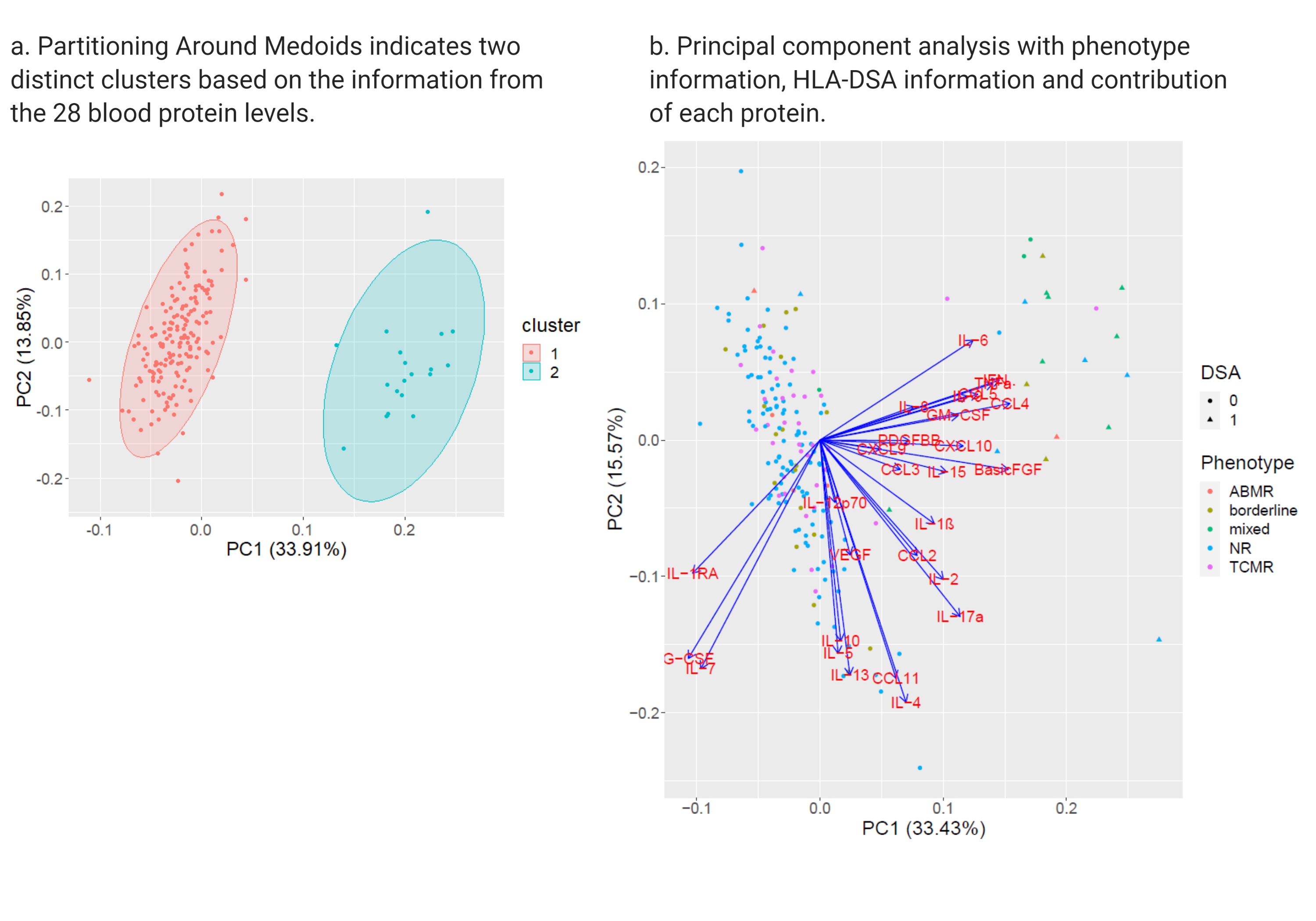
*Methods: Levels of 28 cytokines, chemokines and growth factors were assessed using multiplexed Luminex magnetic bead testing in 293 peripheral blood samples. Blood samples were collected between 2012 and 2016, at time of a kidney allograft biopsy for graft dysfunction within the first year after transplantation in a cohort of 192 consecutive transplants at a single kidney transplant center.
*Results: Principal component analysis and hierarchical clustering uncovered two clusters, distinct in their pro-inflammatory cytokine levels (Figure a). Patients in Cluster I (N=20) had higher pro-inflammatory protein expression compared to patients in cluster II (N=172) and were hallmarked by high prevalence of donor-specific anti-HLA antibodies (HLA-DSA) (N=15/20) (Figure b), and high acute inflammatory histological lesion scores. In 30% (N= 6/20) of biopsies in cluster I, there was no histological evidence of rejection. Cluster I had worse graft survival independent of female sex, repeat transplantation, induction therapy and ongoing histological rejection (adjusted hazard ratio 3.31, 95% CI 1.09 -10.03, p=0.03). The observed inflammatory cytokine profiles were confirmed in in vitro models of DSA-mediated NK cell and/or monocyte activation.
*Conclusions: The expression of pro-inflammatory cytokines is increased in peripheral blood of kidney transplant patients with circulating HLA-DSA, even in the absence of histopathology of rejection. These results challenge the vision that kidney transplant histology is the gold standard for identification of ongoing allo-immune processes.
To cite this abstract in AMA style:
Loon EVan, Barba T, Lamarthée B, Senev A, Thaunat O, Schols D, Naesens M. Peripheral Blood Inflammatory Chemokines Uncover Rejection in the Absence of Histological Lesions [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/peripheral-blood-inflammatory-chemokines-uncover-rejection-in-the-absence-of-histological-lesions/. Accessed January 9, 2026.« Back to 2021 American Transplant Congress