Successful Use of Tedizolid for the Treatment of Nocardiosis in Transplant Recipients
R. Odrobina1, B. Tritle2, C. A.Gomez1
1Division of Infectious Diseases, University of Utah, Salt Lake City, UT, 2Department of Pharmacy, University of Utah, Salt Lake City, UT
Meeting: 2020 American Transplant Congress
Abstract number: D-160
Keywords: Adverse effects, Bacterial infection, Bone marrow transplantation, Infection
Session Information
Session Name: Poster Session D: All Infections (Excluding Kidney & Viral Hepatitis)
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Nocardiosis is an opportunistic infection occasionally seen after solid organ (SOT) and hematopoietic stem-cell transplantation. Treatment is challenging due to the limited number of oral agents, drug intolerance, organism resistance, toxicity and need for prolonged therapy.
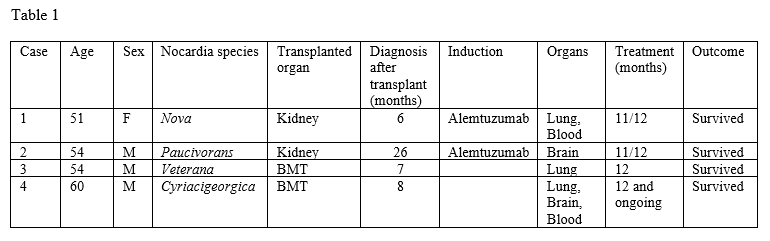
*Methods: Linezolid (LZD) and tedizolid (TZD) both have demonstrated excellent in vitro activity against Nocardia species. However, long-term use of LZD is often prohibited by high rates of hematological and mitochondrial toxicity (ie, myelosuppression, lactic acidosis, and peripheral neuropathy). Conversely, long-term therapy with TZD may be better tolerated, but evidence is scarce. Herein, we report the successful use of long-term TZD as the cornerstone of nocardiosis therapy in four transplant patients. (Table 1).
*Results: A 51-year-old woman underwent a deceased-donor kidney transplantation (KT). Six months later she developed fever, chills, and cough. Imaging showed diffuse, patchy ground-glass opacities with focal consolidation of the left upper lobe. Blood and sputum cultures grew Nocardia nova. She was started on trimethoprim-sulfamethoxazole (TMP-SMX) and LZD. Due to intolerance, she was switched to azithromycin and TZD which she has tolerated well for 11 months into a planned year-long therapy. A 54-year-old male underwent a living, unrelated-donor KT. 26 months after transplant he developed a headache, confusion, and altered gait. Imaging showed a new left occipital brain abscess. Intraoperative cultures grew Nocardia paucivorans. He was initially treated with ceftriaxone and TMP-SMX. Due to hyperkalemia and renal failure, he continued ceftriaxone with TZD with a plan for 1 year of therapy. A 54-year-old male underwent an allogeneic stem cell transplant (SCT). Seven months later he developed a large pleural effusion with cultures positive for Nocardia veterana. He received empiric TMP-SMX and LZD. Due to side effects, his antimicrobials were changed, and he successfully completed treatment with TMP-SMX and TZD. A 60-year-old male underwent allogeneic SCT. Eight months after transplantation he developed fever and cough. Chest imaging revealed numerous pulmonary nodules. Pulmonary and blood cultures grew Nocardia cyriacigeorgica. Initial broad-spectrum antibiotics were changed to TMP-SMX and TZD which he has continued with clinical improvement.
*Conclusions: All patients responded to therapy appropriately and tolerated TZD well. We postulate a potential role of TZD in treatment of nocardiosis in transplant recipients.
To cite this abstract in AMA style:
Odrobina R, Tritle B, AGomez C. Successful Use of Tedizolid for the Treatment of Nocardiosis in Transplant Recipients [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/successful-use-of-tedizolid-for-the-treatment-of-nocardiosis-in-transplant-recipients/. Accessed January 9, 2026.« Back to 2020 American Transplant Congress