Pediatric Liver Transplantation for Metabolic Liver Diseases versus Biliary Atresia: Single Center Experience
A. M. Elsabbagh, K. M. Khan, A. A. Amin, S. S. Kaufman, N. A. Yazigi, T. M. Fishbein
MedStar Georgetown Transplant Institute, Georgetown University Hospital, Washington, DC
Meeting: 2020 American Transplant Congress
Abstract number: D-142
Keywords: Biliary atresia, Liver transplantation, Metabolic disease, Pediatric
Session Information
Session Name: Poster Session D: Liver: Pediatrics
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: The main indication for LT in children has been biliary atresia (BA). Recent advances in surgical management and the development of new immunosuppressants have made LT a viable therapeutic option for an increasing number of disorders in this modern era. In particular LT has become an effective therapeutic modality for metabolic liver diseases, especially urea cycle disorders and maple syrup disease. Patients with metabolic liver diseases are given priority under the PELD system by effectively raising them to ta status where the BA patients would be in ICU (1B). To be considered a treatment of choice for metabolic patients, LT must have at least equivalent outcomes to life saving transplant for BA. As a large center for LT for metabolic disorders we are able to examine this issue.
*Methods: This was a retrospective analysis comparing between isolated pediatric liver transplantation for metabolic liver diseases (N= 62) versus biliary atresia (N= 55) in the period between January 2008 and December 2018.
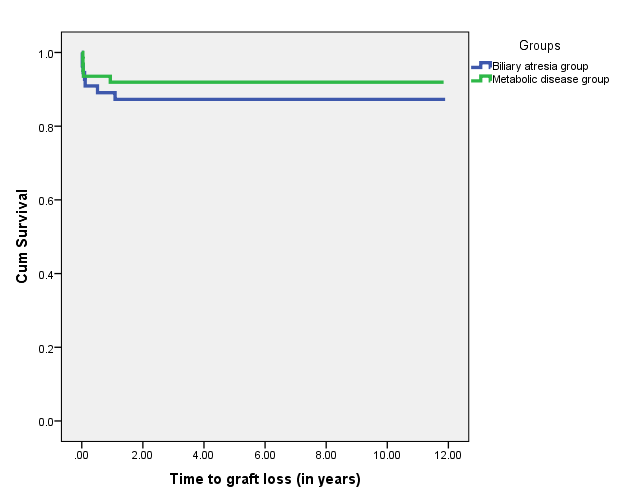
*Results: Median age for the metabolic group was 2 (0.16-16) year versus 1 (0.4-15) year for the BA group (P=0.0001). 41.9 % were female in metabolic group versus 73.6 % in BA group (P = 0.001). 14.5% were African American in the metabolic group versus 41.5% in biliary atresia group (P = 0.010). Graft types included whole liver, cadaveric split liver, living donor segmental liver (54.8%, 38.7%, 6.5% in Metabolic group versus 40%, 27.3%, 32.7% in the BA group, P = 0.001). The 1-, 3-, and 5-year patient survival for metabolic group was 97%, 97%, and 97% versus 96%, 96%, and 96% for the BA group (P = 0.902). The 1-, 3-, and 5-year graft survival for metabolic group was 92%, 92%, and 92% versus 87%, 87%, and 87% for the BA group (P = 0.418). Postoperative complications included biliary (12.9% in metabolic vs. 29.1 % in the BA group, P = 0.030), vascular (14.5% in the metabolic group vs. 32.7 % in the BA group, P = 0.020), postoperative bleeding (6.5% in metabolic group vs. 10.9% in the BA group, P =0.389). Acute rejection tended to be higher in metabolic group (37.1% versus 21.8% in the BA group, P = 0.072).
*Conclusions: Metabolic liver diseases are displacing BA getting more whole liver organ transplant. Pediatric liver transplantation for metabolic liver diseases in our high-volume center has excellent outcomes in comparison to biliary atresia. It has similar patient and graft survival but with less postoperative complications and readmissions. Rejections tended to be higher in metabolic group.
To cite this abstract in AMA style:
Elsabbagh AM, Khan KM, Amin AA, Kaufman SS, Yazigi NA, Fishbein TM. Pediatric Liver Transplantation for Metabolic Liver Diseases versus Biliary Atresia: Single Center Experience [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/pediatric-liver-transplantation-for-metabolic-liver-diseases-versus-biliary-atresia-single-center-experience/. Accessed February 10, 2026.« Back to 2020 American Transplant Congress