Pleural Exosome Mediated Donor Antigen Trafficking Into Mediastinal Lymph Nodes Represents a Novel Pathway of Recipient T Cell Activation in Lung Transplantation
1Surgery, University of Pittsburgh, Pittsburgh, PA, 2Surgery, University of Pennsylvania, Philadelphia, PA, 3New York University, New York, NY, 4Pathology, University of Pennsylvania, Philadelphia, PA, 5Surgery, Yale University, New Haven, CT, 6National Cancer Center Japan, Tokyo, Japan, 7Surgery, Washington University, St. Louis, MO
Meeting: 2020 American Transplant Congress
Abstract number: B-377
Keywords: Allorecognition, Antigen presentation, Lung transplantation, Lymph node
Session Information
Session Name: Poster Session B: Antigen Presentation / Allorecognition / Dendritic Cells
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Studies in lung transplant models suggest that reestablishment of lymphatic continuum of pulmonary allograft via lymphangiogenesis is required for selective trafficking of donor antigen and antigen presenting cells to secondary lymphoid structures such as mediastinal lymph nodes. We proposed than an alternative pathway mediated via exosome transport through pleural lymphatics enables donor antigen trafficking to mediastinal lymph nodes.
*Methods: Left lung from transgenic Wistar rats expressing human CD63-GFP exosomes were transplanted into Lewis recipients (n=13). Mediastinal and mesenteric nodes (day 0 to 8) were analyzed for CD63-GFP. Syngeneic and xenogeneic (pleural fluid of lung transplant patients) exosomes were infused into rat pleural space, and mediastinal nodes were analyzed for antigen accumulation. Nodal lymphocytes were analyzed for T proliferation via FACS using CD4, CD8, and Ki67 antibodies. Pleural fluid exosomes from lung transplant patients (n=5) was analyzed.
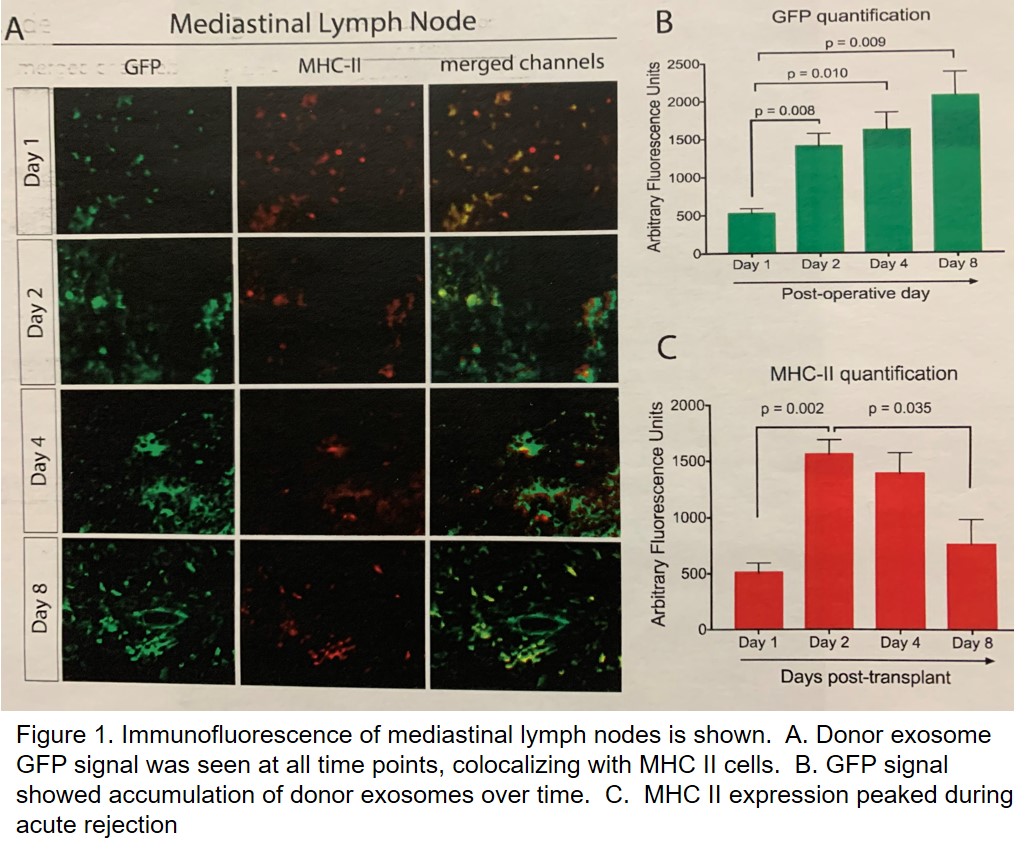
*Results: Selective co-accumulation of CD63-GFP exosome signal with MHC II cells was noted only in mediastinal nodes after transplant, but not mesenteric nodes (Figure 1). This signal was seen at the earliest tested time point of 4 hours post-transplant. Injection of exosomes into rat left pleural space led to selective accumulation of exosome signal only in the ipsilateral and mediastinal lymph nodes at both 12 and 24 hours. FACS for lymphocyte proliferation showed significantly higher proliferation with xenogeneic versus syngeneic exosome injection (p=0.02). Pleural fluid exosomes isolated at 12 to 24 hours after lung transplant showed high levels of donor specific MHC I exosomes in all 5 patients.
*Conclusions: Transplant lung exosomes expressing donor antigen are selectively trafficked to locoregional lymph nodes via the pleural lymphatics, where they can mediate T cell proliferation. This alternative pathway based on pleural transport that is unique to lung transplantation obviates the need for lymphangiogenesis in order to shuttle antigen to locoregional lymph nodes.
To cite this abstract in AMA style:
Habertheuer A, Japp A, Ram C, Chatterjee S, Rostami S, Korutla L, Ochiya T, Naji A, Kreisel D, Vallabhajosyula P. Pleural Exosome Mediated Donor Antigen Trafficking Into Mediastinal Lymph Nodes Represents a Novel Pathway of Recipient T Cell Activation in Lung Transplantation [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/pleural-exosome-mediated-donor-antigen-trafficking-into-mediastinal-lymph-nodes-represents-a-novel-pathway-of-recipient-t-cell-activation-in-lung-transplantation/. Accessed February 17, 2026.« Back to 2020 American Transplant Congress