Predictive Role of the Vitamin B12 in Acute Kidney Injury after Living Donor Liver Transplantation: A Retrospective Observational Cohort Study
St.Mary's Hospital, Seoul, Seoul, Korea, Republic of
Meeting: 2020 American Transplant Congress
Abstract number: B-166
Keywords: Liver transplantation, Post-operative complications, Renal injury
Session Information
Session Name: Poster Session B: Liver: Living Donors and Partial Grafts
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: The aim of our study is to examine the association between serum vitamin B12 level and development of postoperative acute kidney injury (AKI) in patients undergoing living donor liver transplantation (LDLT).
*Methods: The exclusion criteria include preoperative history of kidney dysfunction (i.e., chronic kidney disease, hepatorenal syndrome), history of vitamin B12 supplementation. 109 adult patients were excluded and total 482 adult patients undergoing LDLT were retrospectively investigated. The perioperative recipient and donor-graft findings were compared between the non-AKI and AKI groups using the Mann-Whitney U test, and the χ2 test or Fisher’s exact test. The association between the perioperative factors and AKI was analyzed using univariable and multivariable logistic regression. Overall patient survival in the follow-up period was estimated using Kaplan-Meier test and compared according to AKI occurrence.
*Results: Population of the study was largely male (69.1%) and the median (IQR) of age and BMI were 53 (47.75-50) years and 24.2 (22.3 – 26.7) kg/m2. The etiology for LDLT was as follows: hepatitis B (73%); hepatitis C (9.6%); autoimmune hepatitis (2.9%); hepatitis A (2.3%); drug and toxic hepatitis (1.6%); and cryptogenic hepatitis (10.6%). The median (IQR) MELD score was 14 (9-24). Incidence of AKI development was 24.5 % and median (IQR) follow-up period was 3.9 (1.5 – 7) years.
After an analysis of the potentially valid factors in multivariable logistic regression, the Vitamin B12 (continuous data) was significantly associated with AKI development, together with diabetes mellitus, intraoperative requirement of FFP and hourly urine output (area under curve (AUC): 0.713; 95% CI: 0.664-0.762; p < 0.001 in the predictive model). Furthermore, the probability of AKI development in patients with high vitamin B12 level was higher than in those with normal vitamin B12 level (odds ratio: 2.854; 95% CI: 1.702 - 4.785; p < 0.001)
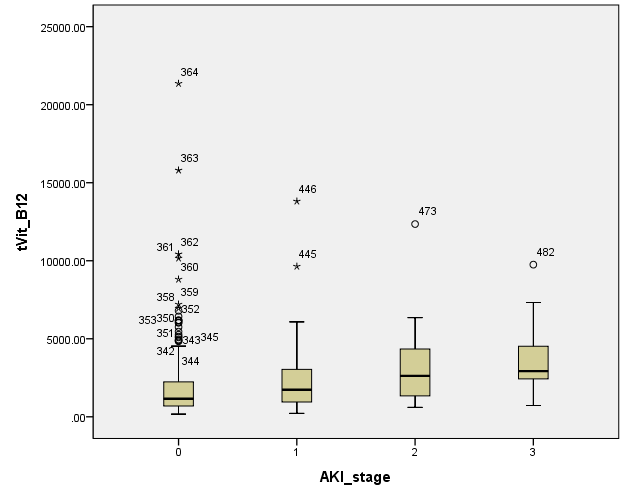
And the higher the AKI stage, the higher the vitamin B12 level.
Also, the AKI group showed worse survival rate than non-AKI group.
*Conclusions: Serum vitamin B12 level is an independent factor in predicting postoperative AKI development in LDLT patients, together with diabetes mellitus, intraoperative requirement of FFP and hourly urine output during. Postoperative AKI is a common complication after LDLT and it is strongly associated with morbidity and mortality. Early assessment of preoperative risk factors, especially vitamin B12, seems to be beneficial for outcome of patients undergoing LDLT.
To cite this abstract in AMA style:
Park J, Chae M. Predictive Role of the Vitamin B12 in Acute Kidney Injury after Living Donor Liver Transplantation: A Retrospective Observational Cohort Study [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/predictive-role-of-the-vitamin-b12-in-acute-kidney-injury-after-living-donor-liver-transplantation-a-retrospective-observational-cohort-study/. Accessed February 24, 2026.« Back to 2020 American Transplant Congress