National Experience with Living Donor Liver Transplant for Hepatocellular Carcinoma
J. Silverstein1, F. Yao1, J. D. Grab2, H. Braun2, J. Roberts2, J. Dodge2, N. Mehta1
1Dept of Medicine, UCSF, San Francisco, CA, 2Dept of Surgery, UCSF, San Francisco, CA
Meeting: 2020 American Transplant Congress
Abstract number: B-161
Keywords: Hepatocellular carcinoma, Liver, Liver transplantation, Living-related liver donors
Session Information
Session Name: Poster Session B: Liver: Living Donors and Partial Grafts
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: LDLT is an attractive option to decrease both wait time and risk of waitlist dropout in HCC. This study aimed to evaluate temporal and regional trends in LDLT utilization for HCC in the United States, and compare the post-LT outcomes with LDLT versus deceased donor liver transplantation (DDLT).
*Methods: Using the UNOS database, we identified 20,161 adult HCC patients who underwent LT from 1998-2018 which included 726 (3.6%) LDLT and 19,435 (96.4%) DDLT at LT centers which performed at least 1 LDLT for HCC.
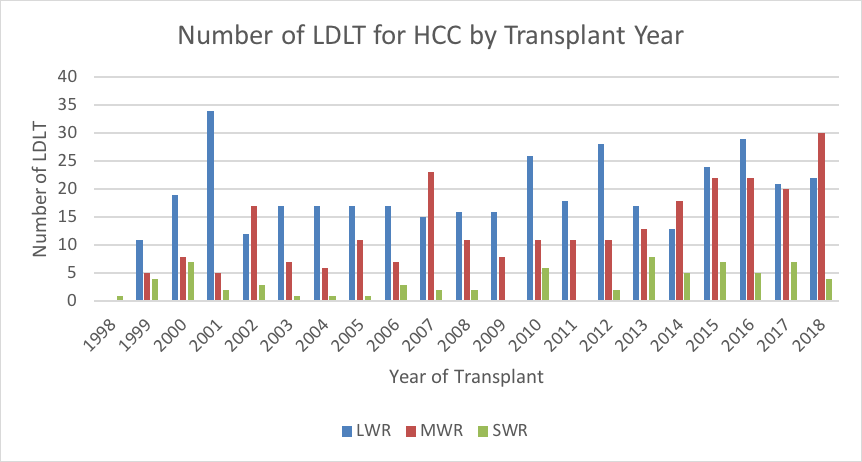
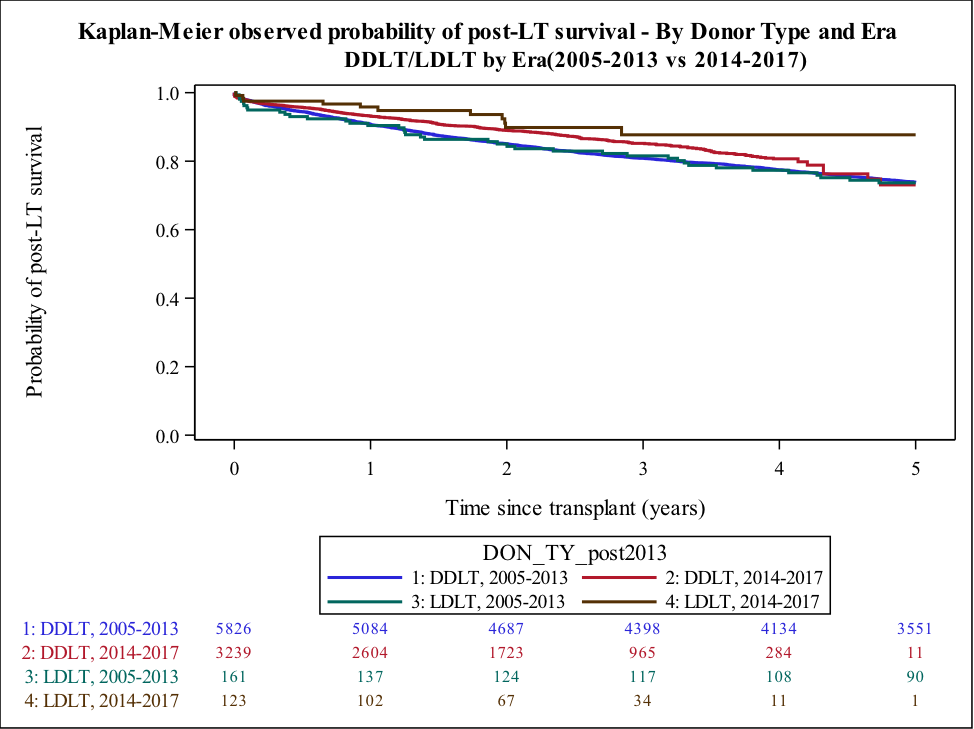
*Results: LDLT utilization was highest prior to the 2002 HCC MELD exception policy, averaging 17.5% of all LT for HCC from 1999-2001. In 2002, usage dropped to 4.4% averaging 3.1% of LT from 2002-2014. Since the institution of a 6-month wait policy in 2015, LDLT for HCC increased from 32/year in 2002-2014 to 53/year in 2015-2018. Long wait regions (1,5,9) utilized LDLT the most but mid wait regions (MWRs: 2,4,6,7,8) had the largest increase from 3.7% before 2015 to 6.0% in 2018 (Figure 1). HCC patients receiving LDLT compared to DDLT were more often female (28% vs 22%) and Caucasian (70% vs 63%) with less African Americans (5% vs 11%) and younger donor age (35 vs 44 years) (all p<0.01). LDLT recipients had larger total tumor diameter (2.3 vs 2.1 cm, p=0.02) and higher AFP (11.5 vs 9.0 ng/ml, p=0.04) at LT but similar MELD and Child-Pugh scores. Wait time was shorter for LDLT (4.2 vs 5.6 months, p<0.001). 5-year post-LT outcomes were similar for LDLT and DDLT, including overall survival (77% vs 75%), graft survival (72% vs 72%) and HCC recurrence (11% vs 13%) (all p>0.20). From 2014-2017, LDLT patients had improved post-LT survival compared to DDLT (Figure 2). On MV analysis, increasing recipient and donor age, total tumor diameter, AFP, MELD, and cold ischemia time were significantly associated with worse post-LT survival whereas receipt of LDLT was not (HR 0.98 vs DDLT, p=0.88).
*Conclusions: Utilization of LDLT for HCC was low from 2002-2014 but has increased slightly since the mandatory 6-month wait policy enacted in 2015, especially in MWRs. We observed excellent post-LT survival with LDLT especially from 2014-2017. Therefore, LDLT appears to be an underutilized but valuable option for HCC patients.
To cite this abstract in AMA style:
Silverstein J, Yao F, Grab JD, Braun H, Roberts J, Dodge J, Mehta N. National Experience with Living Donor Liver Transplant for Hepatocellular Carcinoma [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/national-experience-with-living-donor-liver-transplant-for-hepatocellular-carcinoma/. Accessed February 17, 2026.« Back to 2020 American Transplant Congress