Persistent Fibrinolysis Shutdown in Liver Transplant Recipients is Associated with Early Allograph Dysfunction
1University of Colorado, Aurora, CO, 2Childrens Hospital, Aurora, CO, 3Denver Health Medical Center, Denver, CO
Meeting: 2020 American Transplant Congress
Abstract number: A-307
Keywords: Fibrosis, Liver grafts, Liver preservation, Liver transplantation
Session Information
Session Name: Poster Session A: Biomarkers, Immune Assessment and Clinical Outcomes
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Early allograph dysfunction (EAD) in liver transplantation has been attributed to microvascular thrombosis. Treating grafts at risk of EAD with tissue plasminogen activator (tPA) to lyse presumed clots demonstrated promising resulting in improving graft function. However, a persistent tPA resistant state (fibrinolysis shutdown) in intensive care unit (ICU) patients has been associated with organ failure. This low fibrinolytic state could pose a risk for EAD in liver transplant recipients. We hypothesize that patients that remain in fibrinolysis shutdown following liver transplant will have evidence of EAD.
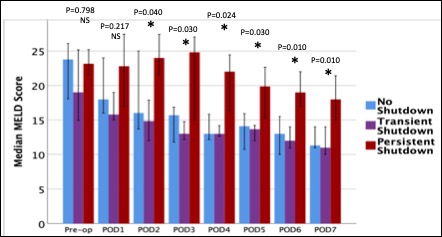
*Methods: Liver transplant recipient samples were obtained pre through post-operative day (POD) 5. Blood was analyzed with thrombelastography (TEG) with exogenous tPA (75 ng/ml) to quantify fibrinolysis resistance [percent clot lysis 30 minutes after maximum clot strength (LY30)]. EAD was defined by A2ALL criteria. An LY30 of < 1.6% (risk factor for ICU organ failure) was used to define fibrinolysis shutdown. Patients were dichotomized on POD 1 shutdown status and further stratified by the duration they remained in shutdown [recovered from shutdown (transient) and remained in shutdown (persistent)]. These three cohorts were contrasted using Kruskall-Wallis test.
*Results: Fifty recipients have complete blood samples for analysis. The median MELD was 21 and early allograph dysfunction (EAD) occurred in 18%. Transient shutdown occurred in 40% of patients, persistent 38%, and no shutdown 22%. There were no differences in pre-operative MELD scores between the cohorts, but the persistent fibrinolysis shutdown retained higher MELD scores starting POD2 (figure). Within the MELD score components, bilirubin was significantly elevated in the persistent group POD3-7, creatinine was increased POD 6-7, and INR was elevated on POD6. EAD increased based on duration of fibrinolysis shutdown (no shutdown 9%, transient 15%, and persistent 26% p=0.216) and was significant when assessing the biliary component of EAD (bilirubin>10 POD7; no 0%, transient 5%, persistent 21% p=0.048).
*Conclusions: Persistent fibrinolysis shutdown in liver transplant recipients is associated with an elevated post-operative MELD and evidence of EAD. Identifying the mechanisms driving this process is an essential step towards understanding this disease process, which may provide therapeutic opportunities to improve graft function following liver transplantation.
To cite this abstract in AMA style:
Moore HB, Nydam T, Pomposelli J, Walker C, Schulick A, Choudhury R, Yaffe H, Adams M, Cohen M, Pomfret E. Persistent Fibrinolysis Shutdown in Liver Transplant Recipients is Associated with Early Allograph Dysfunction [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/persistent-fibrinolysis-shutdown-in-liver-transplant-recipients-is-associated-with-early-allograph-dysfunction/. Accessed January 20, 2026.« Back to 2020 American Transplant Congress