A Multidisciplinary Protocol for the Management of Hyponatremia at the Time of Liver Transplantation is Associated with Reduced Post-Transplant Neurologic Complications
Mount Sinai, New York, NY
Meeting: 2020 American Transplant Congress
Abstract number: 373
Keywords: Liver, Liver transplantation, Neurotoxicity, Outcome
Session Information
Session Name: Liver Retransplantation and Other Complications
Session Type: Oral Abstract Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:45pm
 Presentation Time: 4:03pm-4:15pm
Presentation Time: 4:03pm-4:15pm
Location: Virtual
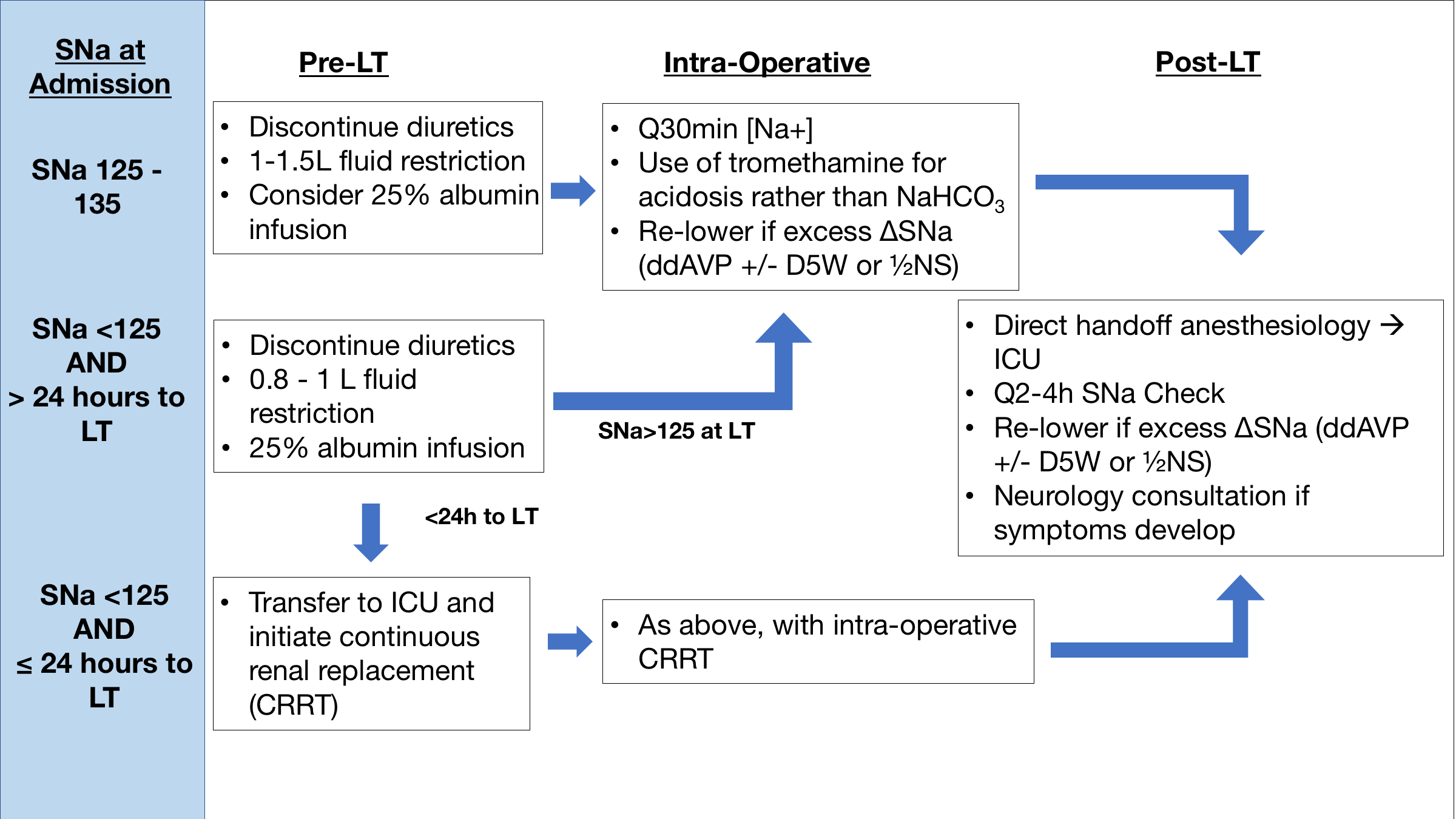
*Purpose: The primary purpose of this study was to assess whether implementation of a multidisciplinary protocol (Figure 1) aimed at limiting rapid changes in serum sodium (SNa) peri-liver transplant (LT) impacted rates of neurologic complications (NCs) post-LT.
*Methods: A retrospective review of adult patients who underwent LT at the Mount Sinai Hospital from 1/2016-10/2017 was performed. Patients who were hyponatremic (SNa<135 mEq/L) within 7 days of LT were analyzed in two eras: Era 1 (pre-protocol, 1/2016-10/2016) and Era 2 (post-protocol, 10/2016-10/2017). Perioperative change in serum sodium from LT to 24-hours post-LT (deltaSNaLT) was calculated. The primary outcome was the development of NCs within 3 months post-LT. Multivariable logistic regression was performed to assess for independent association between eras and the development of NCs.
*Results: A total of 89 and 114 patients underwent LT in Era 1 and Era 2, of whom 42 (47.2%) and 45 (39.5%) were hyponatremic within 7 days of LT, respectively. There were no significant differences in patient age, sex, ethnicity, or etiology of liver disease at baseline. Median SNa was similar between the eras immediately pre-LT (133 mEq/L [interquartile range (IQR) 130-135] vs. 133 [IQR 129-135.5], p=0.84). A significantly greater proportion of patients in Era 1 developed deltaSNaLT>10 mEq/L (28.6% vs. 8.9%, p=0.02) and deltaSNaLT>12 mEq/L (21.4% vs. 4.4%, p=0.02). A significantly greater proportion of patients in Era 1 developed post-LT NCs vs. Era 2 (35.7% vs. 13.3%, p=0.01). The most common NC was persistent altered sensorium (43% of total CNs). Osmotic demyelination developed in 2 patients in Era 1 and none in Era 2 (p=0.14). When controlling for baseline group differences, multivariable logistic regression revealed that Era 2 was associated with significantly reduced odds (odds ratio [OR] 0.27, 95% confidence interval [CI] 0.08-0.86) of developing NCs, while deltaSNaLT>12 mEq/L was associated with higher odds of developing NCs (OR=4.7, 95%CI 1.1-20.4).
*Conclusions: Transplantation during Era 2 was independently associated with significantly reduced odds of developing NCs. Standardization of the management of peri-LT hyponatremia may lead to improved neurologic outcomes post-LT.
To cite this abstract in AMA style:
Crismale JF, Huisman T, Deshpande R, Law C, Im G, Bronster D, Jr SDemaria, Florman S, Schiano T. A Multidisciplinary Protocol for the Management of Hyponatremia at the Time of Liver Transplantation is Associated with Reduced Post-Transplant Neurologic Complications [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/a-multidisciplinary-protocol-for-the-management-of-hyponatremia-at-the-time-of-liver-transplantation-is-associated-with-reduced-post-transplant-neurologic-complications/. Accessed January 30, 2026.« Back to 2020 American Transplant Congress