The Perioperative Coagulation Profile of Hepatocellular Carcinoma During Liver Transplantation Compared to Patients with Non-Malignant Disease: A Cause or Association for Decreased Blood Product Utilization During Liver Transplantation?
University of Colorado, Aurora, CO
Meeting: 2020 American Transplant Congress
Abstract number: 256
Keywords: Blood transfusion, Hepatocellular carcinoma, Liver, Liver transplantation
Session Information
Session Name: Liver: Hepatocellular Carcinoma and Other Malignancies II
Session Type: Oral Abstract Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:45pm
 Presentation Time: 4:27pm-4:39pm
Presentation Time: 4:27pm-4:39pm
Location: Virtual
*Purpose: Hepatobiliary malignancies have been associated with hyper-coagulability. However, the impact of hepatocellular carcinoma (HCC) on coagulation during liver transplantation remains less clear. We hypothesize that patients with HCC have a distinct perioperative coagulation profile compared to patient’ with nonmalignant disease during liver transplantation.
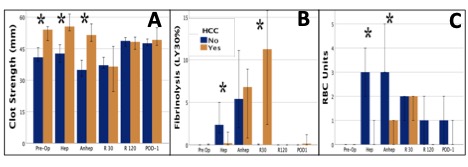
*Methods: Liver transplant recipients underwent serial perioperative blood samples [pre-op, hepatectomy, anhepatic, early reperfusion (30 min), late reperfusion (120 min), and post operative day 1 (POD-1)]. Blood was analyzed with thrombelastography (TEG) to quantify clot strength (MA) and fibrinolysis (LY30). Patients were dichotomized on HCC status. Coagulation variables and blood products were compared between cohorts with a Mann Whitney U test.
*Results: 100 patients were included (24% HCC). HCC patients had lower MELDs (11 vs 24 p<0.001) decreased INR (1.4 vs 2.1 p<0.001) and higher platelet counts (74 vs 54 p<0.092). HCC patients had increased clot strength at baseline and through the anhepatic phase of surgery (P<0.006 for all Panel A), but clot strength was not significant after graft reperfusion. Fibrinolytic activity was decreased in patients with HCC at the anhepatic phase of surgery (p=0.026) but became markedly increased during early reperfusion (p=0.003 Figure Panel B). Red blood cell transfusions ([RBC (panel C)] were reduced in patients with HCC until reperfusion (p<0.000 all) which equated to 5X less transfusions during this time (2 vs 10 units p<0.001). RBC transfusions inversley correlated with clot strength (Spearman’s Rho -0.336 p<0.001). When controlling for INR and platelet count, HCC persisted as a predictor of lower blood product utilization prior to graft implantation (p=0.020) but lost significance after graft reperfusion (p=0.115).
*Conclusions: HCC was associated with a higher clot strength than patients with non-malignant liver disease, which persisted until early graft reperfusion. While HCC was associated with less severe liver disease, red blood cell transfusions were 5-fold lower and remained significant after adjusting for conventional coagulation assays. Ongoing investigation is warranted to determine if increasing clot strength in nonmalignant liver disease prior to reperfusion to the level of patients with HCC can reduce blood loss without risking thrombotic complications.
To cite this abstract in AMA style:
Moore HB, Pomfret E, Pomposelli J, Walker C, Choudhury R, Yaffe H, Wachs M, Bak T, Conzen K, Adams M, Pshak T, Nydam TL. The Perioperative Coagulation Profile of Hepatocellular Carcinoma During Liver Transplantation Compared to Patients with Non-Malignant Disease: A Cause or Association for Decreased Blood Product Utilization During Liver Transplantation? [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/the-perioperative-coagulation-profile-of-hepatocellular-carcinoma-during-liver-transplantation-compared-to-patients-with-non-malignant-disease-a-cause-or-association-for-decreased-blood-product-utili/. Accessed February 16, 2026.« Back to 2020 American Transplant Congress