The Impact of a Positive Crossmatch on KAS Patients and Organs
1Medical Affairs, Hansa Biopharma, Camas, WA, 2Hansa Biopharma, Lund, Sweden, 3UNOS, Richmond, VA
Meeting: 2020 American Transplant Congress
Abstract number: 236
Keywords: HLA antibodies, HLA antigens, HLA matching, Ischemia
Session Information
Session Name: Kidney Deceased Donor Allocation II
Session Type: Oral Abstract Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:45pm
 Presentation Time: 4:27pm-4:39pm
Presentation Time: 4:27pm-4:39pm
Location: Virtual
*Purpose: Evaluate the potential effects of offer refusals due to positive crossmatch (+XM) on both patients and re-allocated organs with a focus on waitlist outcomes, organ cold ischemia times (CIT), and discarded kidney rate.
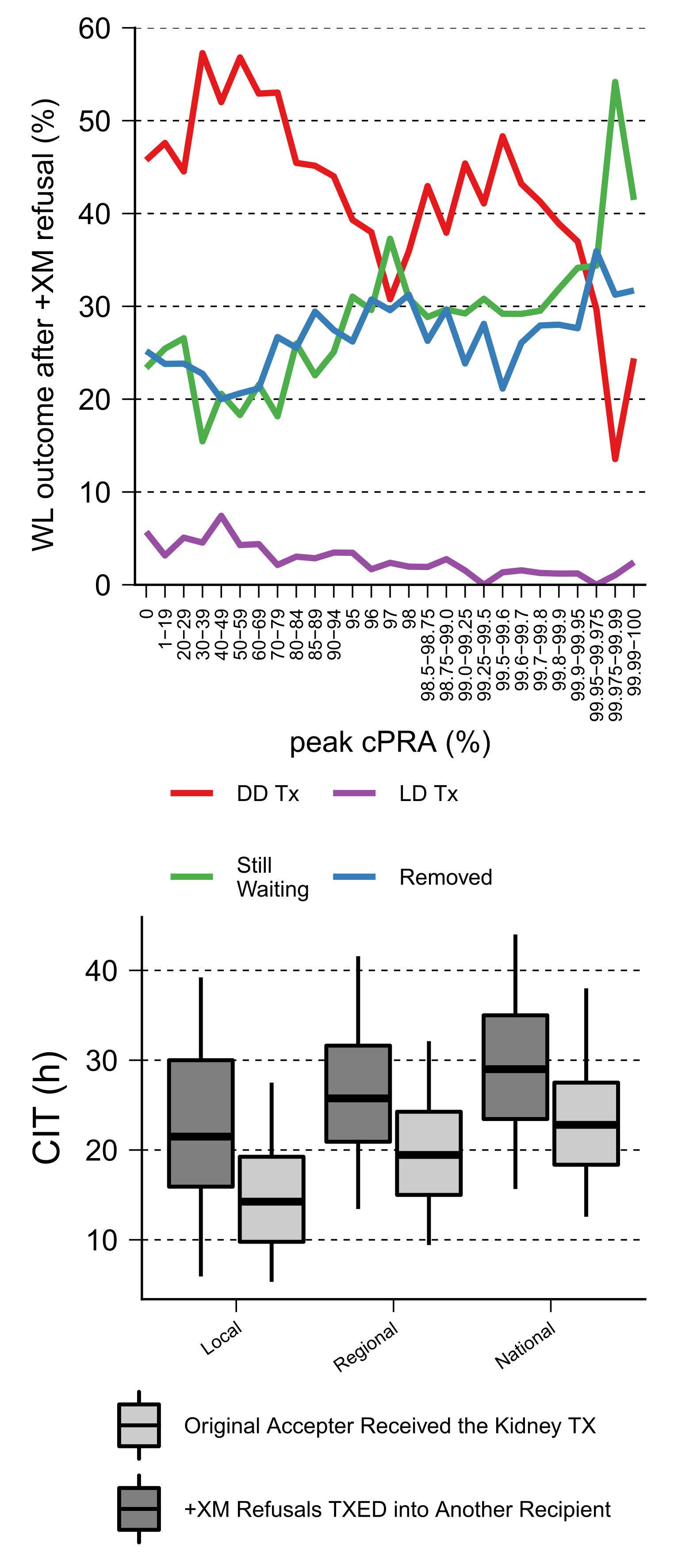
*Methods: Organ Procurement and Transplantation Network deceased donor kidney transplant (DDKT) waitlist data from 2015-2018 were assessed for patient and kidney outcomes after a +XM. Waitlist registrants were stratified into 27 cPRA groups. Post +XM waitlist registrants were evaluated for their current waitlist status (as of 10/11/2019). Kidneys reallocated after a positive crossmatch were evaluated for discard rate and changes in CIT to new recipients.
*Results: Kidney match runs over the time period resulted in 17,741 +XM refusals, of which 3,989(22.5%) had a cPRA of ≥99.5%. Waitlist Outcomes after a +XM: Among all waitlisted kidney transplant candidates with a first time +XM refusal (n=9,317) during 2015-2018, 45% (n=4,142) received a DDKT, 26.1% (n=2,428) were currently listed as still waiting, and 25.9% (n=2,415) were removed from the waitlist for either death, too sick, or other, as of 10/11/2019. Patients with +XM refusals and a cPRA ≥99.9% (n=511) 30% (n=152) received a DDKT and 39% (n=197) were still waiting. Furthermore, by combining the outcomes of those removed from waitlist (death, too sick, or other) 31% (n=157) ended up delisted after a +XM refusal. Kidneys Refused for a +XM Among kidneys reallocated (n=930) after an offer was accepted and later refused due to a +XM, 84 (9%) were discarded while the remainder 846 (91%) were allocated to a different recipient. CIT was increased in kidneys transplanted in another waitlist registrant after a +XM compared to kidneys placed with original acceptor. The median CIT increase for local, regional and nationally reallocated kidneys after a +XM were 7.2, 6.3, and 6.2 hours respectively.
*Conclusions: Reallocating kidneys due to +XM affects organ allocation by significantly increasing CIT and resulting in the discard of approximately 25 kidneys annually. Patients were affected with longer waiting times and a significant number ending up dying or being delisted. Furthermore, markedly fewer patients with cPRA ≥99.9 experiencing a +XM refusal received a transplant (30%) compared to other +XM refusal waitlist patients (45%). Technologies and therapies to reduce +XM refusals could potentially have a positive impact on patients and allocation.
To cite this abstract in AMA style:
Lee J, Sjöholm K, Kjellman C, Lorant T, Winstedt L, Nigro V, Roupé KM, Schiött Å, Runstrom A, Taranto S, Baker T, Stewart D. The Impact of a Positive Crossmatch on KAS Patients and Organs [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/the-impact-of-a-positive-crossmatch-on-kas-patients-and-organs/. Accessed February 5, 2026.« Back to 2020 American Transplant Congress