Effects of Mandatory 6-Month Waiting Time Policy on Post-Transplant Outcomes and Explant Pathology in Liver Transplant Patients with Hepatocellular Carcinoma
Henry Ford Hospital, Detroit, MI
Meeting: 2020 American Transplant Congress
Abstract number: 146
Keywords: Allocation, Hepatocellular carcinoma, Histology, Liver transplantation
Session Information
Session Name: Liver: Hepatocellular Carcinoma and Other Malignancies I
Session Type: Oral Abstract Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:45pm
 Presentation Time: 3:39pm-3:51pm
Presentation Time: 3:39pm-3:51pm
Location: Virtual
*Purpose: In the United States, current allocation policy mandates a 6-month waiting period before exception scores are granted to liver transplant (LT) candidates with hepatocellular carcinoma (HCC). This study aims to determine if this delay led to an improvement in post-transplant outcomes in HCC patients by negative selection of biologically aggressive tumors.
*Methods: We examined two groups from the UNOS registry; Group 1 (pre 6-month rule) comprised LT recipients registered as transplant candidates with HCC exception scores from Jan. 1, 2013 to Oct. 7, 2015 (n=3,024). Group 2 (post 6-month rule) comprised LT patients with HCC registered from Oct. 8, 2015 to Jun. 30, 2018 (n=2,249). Patients were compared for HCC directed therapy, explant histology and post-LT patient and graft survival and mortality from cancer.
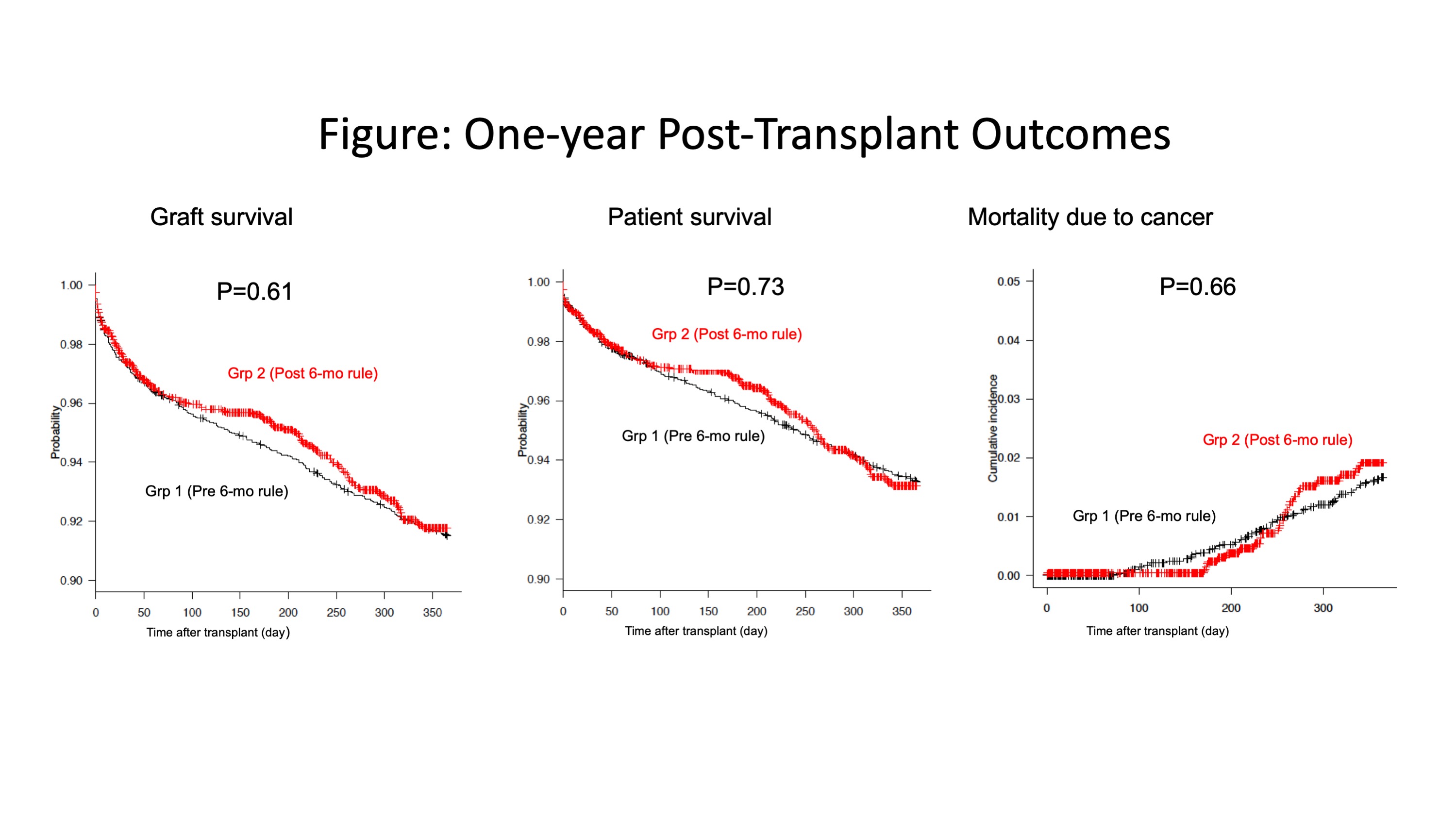
*Results: The six month delay in granting HCC exception points led to a significant decline in patients receiving LT in the first six months after listing (Group 2 vs Group 1: 6.3% vs 42%: P<0.001). However, in comparing Group 2 vs Group 1, there were no differences in one year post-transplant patient (93.1% vs. 93.2%: aHR 0.99, 95%CI 0.77-1.27) or graft survival (91.8% vs. 91.5%: aHR 0.98, 95%CI 0.78-1.22). In addition, the one-year incidence rate of mortality due to malignancy was comparable between groups (P=0.66). Patients in Group 2 (post 6-month rule) were more likely to have received HCC directed therapy on the waiting list than in Group 1 (97.7% vs. 92.1%: P<0.001) and were more likely to have received microsphere therapy (12.3% vs. 5.4%: P<0.001). In Group 2 vs. Group 1, there were no differences, on explant pathology, in multifocal disease (47.9% vs. 45.6%), HCC within Milan criteria (70.3 vs. 72.1%), vascular invasion (15.2% vs. 15.1%) or extrahepatic disease (2.6% vs. 2.9%). However, patients in Group 2 were more likely to have complete necrosis (24.8% vs. 19.2%: P<0.001) and a lower alpha-fetoprotein at transplant (33.1 + 172 vs. 69.7 + 526: P<0.001). Recipient older age, lower functional status, explant tumor exceeding Milan criteria, poorly differentiated HCC, older donor age, and donation after cardiac death donor were independent risk factors for one-year patient mortality.
*Conclusions: The six month waiting rule did lead to a decline in LT in the first six months after listing. However, there were no differences in post-transplant patient survival or mortality from recurrent cancer. Patients in the 6-month delay period were more likely to have received HCC directed therapy and have complete necrosis on explant.
To cite this abstract in AMA style:
Nagai S, Kitajima T, Yeddula S, Salgia R, Abouljoud M, Moonka D. Effects of Mandatory 6-Month Waiting Time Policy on Post-Transplant Outcomes and Explant Pathology in Liver Transplant Patients with Hepatocellular Carcinoma [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/effects-of-mandatory-6-month-waiting-time-policy-on-post-transplant-outcomes-and-explant-pathology-in-liver-transplant-patients-with-hepatocellular-carcinoma/. Accessed February 19, 2026.« Back to 2020 American Transplant Congress