Anti-Thymocyte Globulin versus Interleukin-2 Receptor Antagonist and Deceased-Donor Kidney Transplant Outcomes among Older Recipients
1Johns Hopkins University, Baltimore, MD, 2Saint Louis University, St. Louis, MO, 3Drexel University, Philadelphia, PA
Meeting: 2020 American Transplant Congress
Abstract number: 11
Keywords: Efficacy, Elderly patients, Induction therapy, Kidney transplantation
Session Information
Session Name: Kidney Immunosuppression: Induction Therapy
Session Type: Oral Abstract Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:45pm
 Presentation Time: 4:27pm-4:39pm
Presentation Time: 4:27pm-4:39pm
Location: Virtual
*Purpose: Kidney transplantation (KT) has been growing treatment option for older end-stage renal disease patients. Although lymphocyte-depleting agents are considered to be superior than interleukin-2 receptor antagonist showing a reduced risk of rejection in general, there is sparse research on the choice of induction immunosuppressants for older KT recipients. Older recipients experience a compromised immune response due to aging so that specific induction treatment strategy is required. Therefore, we aim to compare the association of rabbit anti-thymocyte globulin (rATG) (versus basiliximab) and KT outcomes between older (≥65 years) and younger (<65 years) KT recipients.
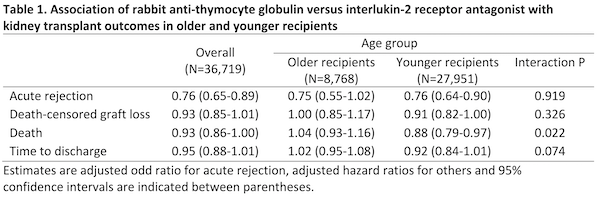
*Methods: Using the United States Renal Data System, we identified 36,719 first-time KT recipients (age ≥18) between January 1, 2010 and December 31, 2016 who received maintenance immunosuppression of tacrolimus, mycophenolate mofetil and steroid at the time of discharge. We estimated adjusted odds ratio (OR) of acute rejection (AR) at 1-year post-KT and hazard ratios (HR) of death-censored graft failure (DCGF) and post-KT mortality by using logistic and Cox regression. Relative time to discharge was tested with accelerated failure time model. All models were weighted by using propensity score to adjust for confounders. We studied effect measure modification by age using a Wald test.
*Results: Of the 36,719 recipients, 72.8% received rATG and 27.2% received basiliximab. Overall, rATG was associated with lower odds of AR at 1-year post-KT (OR 0.76, 95% CI 0.65-0.89, p < 0.001) than basiliximab and the association was not modified by age. Compared with basiliximab, risk of mortality associated with rATG was lower among younger KT recipients (HR 0.88, 95% CI 0.79-0.97, p = 0.008) but not differ among older recipients (HR 1.04, 95% CI 0.93-1.16, p = 0.466; interaction p = 0.022). There was no significant evidence that rATG had better beneficial effects on DCGF (HR 0.93, 95% CI 0.85-1.01, p = 0.081; interaction p = 0.326) and time to discharge (HR 0.95, 95% CI 0.88-1.01, p = 0.101; interaction p = 0.074) compared to basiliximab.
*Conclusions: Among older KT recipients, rATG may reduce the risk of AR compared to basiliximab but may not increase the other three undesirable outcomes. Choice of induction immunosuppression should be tailored by recipient age.
To cite this abstract in AMA style:
Ahn J, Bae S, Lentine K, Schnitzler M, Hess G, Segev D, McAdams-DeMarco M. Anti-Thymocyte Globulin versus Interleukin-2 Receptor Antagonist and Deceased-Donor Kidney Transplant Outcomes among Older Recipients [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/anti-thymocyte-globulin-versus-interleukin-2-receptor-antagonist-and-deceased-donor-kidney-transplant-outcomes-among-older-recipients/. Accessed February 18, 2026.« Back to 2020 American Transplant Congress