Liver Transplantation in Acute Hepatic Insufficiency Induced by Imatinib
1GI Surgery/Transplant, Hospital Samaritano de Sao Paulo, Sao Paulo, Brazil, 2GI Surgery/Transplant, Faculdade de Ciências Médicas da Santa Casa de São Paulo, Sao Paulo, Brazil, 3Faculdade de Ciências Médicas da Santa Casa de São Paulo, Sao Paulo, Brazil
Meeting: 2019 American Transplant Congress
Abstract number: C298
Keywords: Graft survival, Hepatitis, Liver transplantation, Outcome
Session Information
Session Name: Poster Session C: Liver: MELD, Allocation and Donor Issues (DCD/ECD)
Session Type: Poster Session
Date: Monday, June 3, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: Case report of a Woman, pediatrician, 40 yo,with chronic myeloid leukemia using Imatinib who developed Serious Acute Hepatic Failure and needed liver transplant to survive.
*Methods: Case reporting the sequence of events who led to liver transplant and post operative care of a very sick patient.
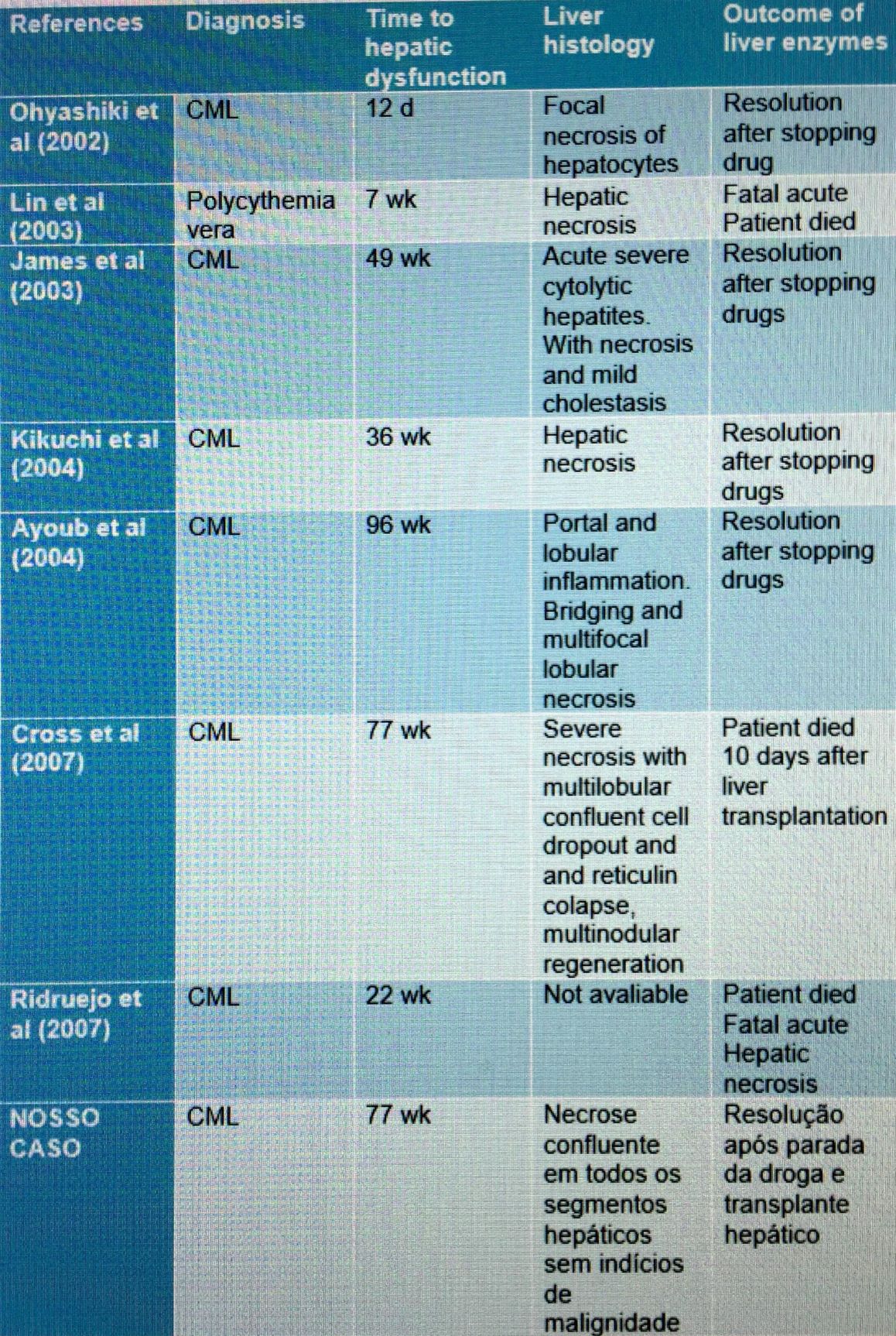
*Results: AMM, female, 40 years old, with chronic myeloid leukemia (CML), in use of Imanitibe 400 mg / day since the diagnosis of the disease on 06/13/2016 and Zolpidem, was hospitalized on 01/21/2018, with a history of jaundice, nausea and vomiting in large quantities a week ago. Patient had previous infection with Cocksakie virus 4 months ago; performed bariatric surgery in 2008; denied use of Paracetamol. At physical examination, he was slow, lethargic, icteric (1 + / 4 +), dehydrated (2 + / 4 +). She presented with abdominal moderate distension, ascites, palpable liver 2 cm from costal border, regular perfusion and discreet Flapping. At admission, the use of Imatinib was discontinued.The following results were obtained: Ammonia of 200 mg / dL (normal parameter: less than 100 mg / dL), INR of 3.2, AST of 1420 (normal parameter: 5-40 units / L), ALT of (Normal parameter: 7-56 units / L), platelets of 84,000 μl (normal parameter: 150,000-400,000 μl), fibrinogen of 170 mg / dL (normal parameter: 195 to 365 mg / dl), and factor V of 29 %. Negative serology for hepatitis A, B and C. In the ultrasound of the total abdomen, the liver had a small size, but with a prominent right lobe, serrated contours and a diffusely heterogeneous texture suggestive of severe parenchymal liver disease. On a previous ultrasound of October 2017, the liver was normal, suggesting acute hepatic involvement.After 6 days of hospitalization, the patient was diagnosed with severe acute liver failure, with 4 + / 4 + icteric and bilirubin of 5.41 g / dL, albumin of 2.8, INR of 4.1, moderate ascites, serum creatinine of 0.7mg / dL, without neurological motor deficits and positive flapping and lowering of the level of consciousness. Patient was promptly submitted to plasmapheresis (PRISMA) and, because they fulfilled criteria of Clinchy – factor V less than 30% in patients over 30 years old, hepatic transplantation was indicated.Transplantation was performed 13 days after hospitalization with cadaveric donor liver with encephalic death, with warm ischemia time of 33 minutes and total ischemia time (cold + warm) of 7 hours and 13 minutes. The procedure was performed without intercurrences. In the surgical pathology, confluent necrosis was found in all hepatic segments and nodules of remaining hepatocytes in segments III, IV and VIII. After surgery, the patient continued to use PRISMA and the patient had a Meld of 37. After 20 days of surgery, a new approach was required for drainage and cleaning of subcutaneous infection with secretion and control of bleeding with aspiration of hematic ascites. Patient progressed steadily and was discharged after 34 days.
*Conclusions: Imatinib is a risk for patients to develop severe acute hepatic failure. Continuous hemodyalisis (PRISMA) is an important tool to keep these patients. Liver transplant may be necessary to save them.
To cite this abstract in AMA style:
David AI, Fantauzzi MC, Santi TDi, Confuorto NC, Martinho GT, Antunes PS. Liver Transplantation in Acute Hepatic Insufficiency Induced by Imatinib [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/liver-transplantation-in-acute-hepatic-insufficiency-induced-by-imatinib/. Accessed February 7, 2026.« Back to 2019 American Transplant Congress