Cholecystitis in High-Acuity Patients Undergoing Liver Transplantation: A Five-Year Analysis of Incidence, Causes and Impact
Dumont-UCLA Liver Transplant Center, Department of Surgery, UCLA School of Medicine, Los Angeles, CA
Meeting: 2019 American Transplant Congress
Abstract number: A362
Keywords: Adverse effects, High-risk, Liver, Risk factors
Session Information
Session Name: Poster Session A: Transplant Infectious Diseases
Session Type: Poster Session
Date: Saturday, June 1, 2019
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall C & D
*Purpose: While the incidence of gallbladder pathology is well described in the general population, there is almost no data on cholecystitis in liver transplant candidates (LTC). We sought to examine the incidence impact, and potential causes of gallbladder pathology on LTC at time of liver transplantation (LT) in a high-acuity patient cohort.
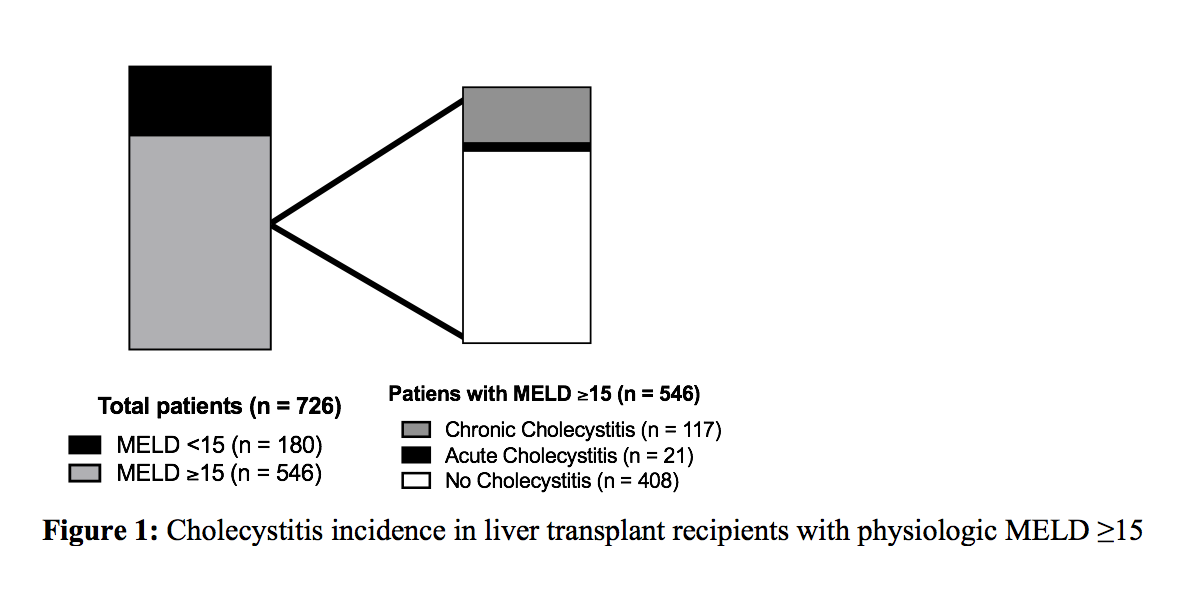
*Methods: All adult LTC undergoing LT at our institution from January 1, 2012 to December 31, 2016 were included. Physiologic Model for End Stage Liver Disease (MELD) at the time of transplant was calculated, and patients with MELD >15 were analyzed. Surgical pathology reports were examined for the presence or absence of acute or chronic cholecystitis. Chi-Square and Mann-Whitney U tests were utilized for comparison. Multivariate analyses were performed to identify factors associated with the incidence of acute or chronic cholecystitis. Graft and patient survival were calculated using the Kaplan Meier method.
*Results: 726 patients underwent primary LT during the study period; 546 patients had a MELD >15. Of these, 405 had surgical pathology that included gallbladder findings. 138 (34%) patients had cholecystitis [chronic cholecystitis n=117 (28%), acute cholecystitis n=21 (5%)] (Figure1). Diabetes was associated with cholecystitis of any type on univariate and multivariate analyses. Total length of stay (LOS), pre-operative white blood cell count (WBC), sepsis within 10 days prior to LT, and location (home vs. floor vs. ICU) prior to transplant were associated with acute cholecystitis on univariate analysis. Total LOS and WBC were associated with acute cholecystitis on multivariate analysis. There was no difference in 12-month overall graft or patient survival.
*Conclusions: Cholecystitis is under-recognized in high-MELD LTC. LTC candidates developing acute cholecystitis are predisposed to having higher overall LOS and elevated WBC pre-LT. While these findings did not impact survival, they potentially contribute to cost and morbidity. Increased awareness, diagnosis, and prompt management of cholecystitis pre-LT may reduce morbidity and optimize care in high acuity patients awaiting LT.
To cite this abstract in AMA style:
Graham DS, Ito T, Lu MM, DiNorcia J, Agopian VG, Yersiz H, Farmer DG, Busuttil RW, Kaldas FM. Cholecystitis in High-Acuity Patients Undergoing Liver Transplantation: A Five-Year Analysis of Incidence, Causes and Impact [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/cholecystitis-in-high-acuity-patients-undergoing-liver-transplantation-a-five-year-analysis-of-incidence-causes-and-impact/. Accessed March 4, 2026.« Back to 2019 American Transplant Congress