Outcomes of En Bloc Simultaneous Liver-Kidney Transplantation Compared to the Traditional Technique
University of Cincinnati, Cincinnati, OH
Meeting: 2019 American Transplant Congress
Abstract number: A292
Keywords: Graft function, Kidney/liver transplantation, Liver transplantation, Surgical complications
Session Information
Session Name: Poster Session A: Liver - Kidney Issues in Liver Transplantation
Session Type: Poster Session
Date: Saturday, June 1, 2019
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall C & D
*Purpose: Simultaneous liver-kidney transplantation (SLKT) is indicated for patients with end-stage liver disease (ESLD) and concurrent renal insufficiency. En bloc SLKT has been reported as an alternative approach to the traditional method of separate implantation of the liver and kidney, but outcomes have not been well studied.
*Methods: All patients who underwent SLKT from 2013 to 2017 at our institution were reviewed. Prior to 2016, SLKT was performed by separate implantation of the liver and kidney through either a single Chevron incision or separate Gibson incision. In 2016, our group adopted the en bloc SLKT technique performed through a single Chevron incision, with renal outflow maintained through the donor infrahepatic vena cava and inflow via anastomosis of the donor renal artery to donor splenic artery. Primary outcomes were kidney delayed graft function (DGF) and graft survival at 1 year.
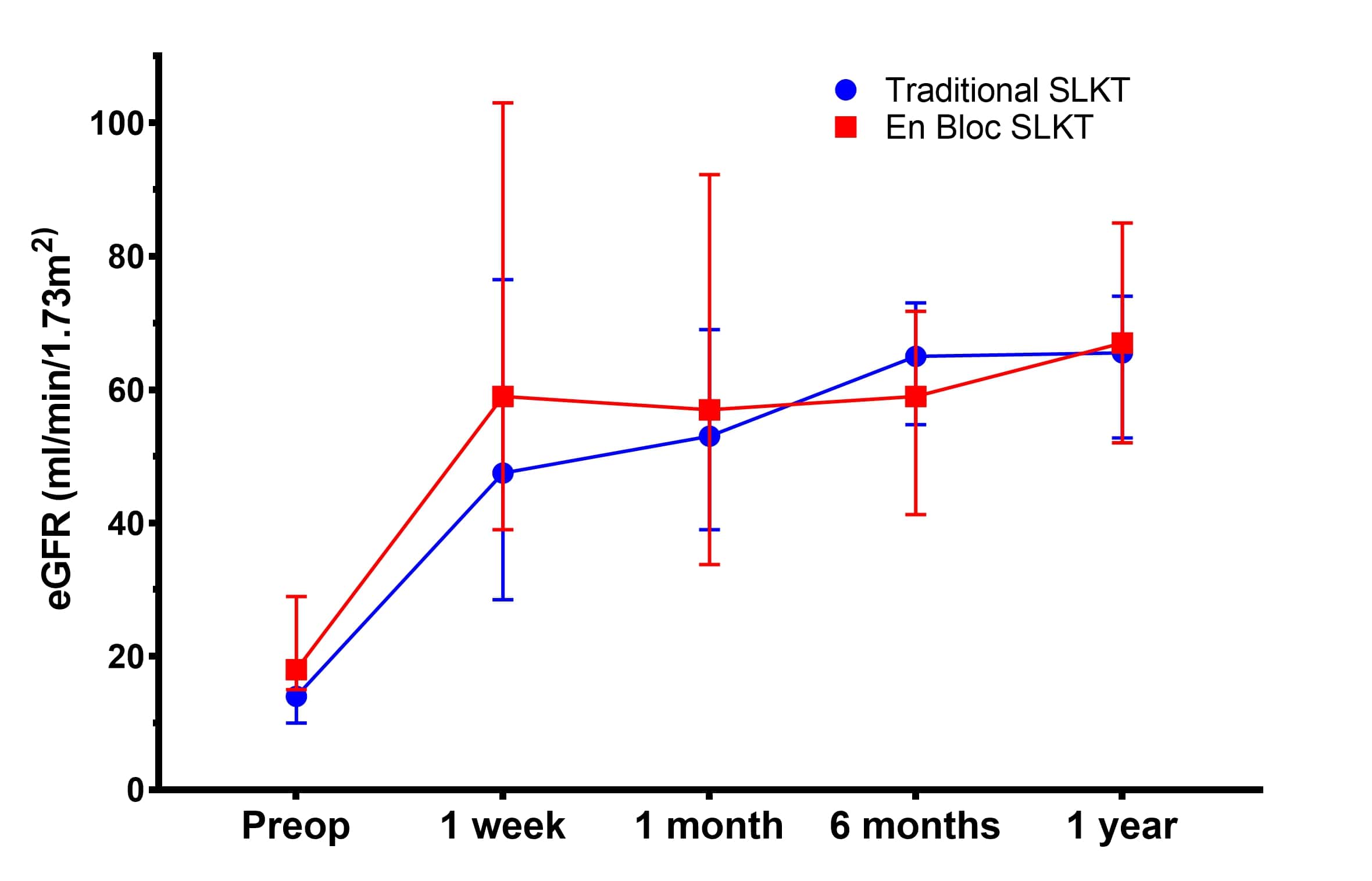
*Results: During the study period, 437 liver transplantations occurred and 34 (7.8%) were SLKT (17 traditional and 17 en bloc). Patients were similar with regard to age, gender, etiology of liver disease, and medical history (all p>0.05). One patient, deemed not a candidate at other centers due to severe iliac atherosclerotic disease, was able to be transplanted using the en bloc technique. Among the en bloc group, renal insufficiency was more commonly the result of ESLD (64.7% vs 29.4%, p=0.03). More patients in the traditional group were on dialysis (82.4% vs 41.2%, p=0.01) and had lower baseline eGFR (14 vs 18, p=0.01) prior to transplant. En bloc SLKT was associated with shorter kidney cold ischemia time (341 vs 533 min, p<0.01) and operative time (374 vs 511 min, p<0.01). Two en bloc patients (11.8%) underwent reoperation for problems with allograft inflow due to kinking (n=1) and renal steal (n=1). Postoperatively, the en bloc group had equal rates of DGF compared to the traditional group (23.5% for both, p=1.0). One-year kidney graft survival was similar between the groups (88.2% vs 82.4%, p=1.0), and both cohorts showed similar improvements in eGFR following transplantation (FIGURE).
*Conclusions: The en bloc technique is a feasible and safe technical variant for SLKT and is associated with comparable outcomes to the traditional method. In our experience, en bloc SLKT was associated with shorter cold ischemia times and, in selected patients, may be the preferred approach.
To cite this abstract in AMA style:
Cortez AR, Lee TC, Kassam A, Morris MC, Winer LK, Silski LSage, Cuffy MC, Diwan TS, Quillin RC, Shah SA. Outcomes of En Bloc Simultaneous Liver-Kidney Transplantation Compared to the Traditional Technique [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/outcomes-of-en-bloc-simultaneous-liver-kidney-transplantation-compared-to-the-traditional-technique/. Accessed February 19, 2026.« Back to 2019 American Transplant Congress