Transcriptional Changes in PBMC Associated with Development of Infection and Rejection in Older and Younger Kidney Transplant Recipients
1Division of Infectious Diseases, David Geffen School of Medicine at UCLA, Los Angeles, CA, 2Department of Pathology and Laboratory Medicine, David Geffen School of Medicine at UCLA, Los Angeles, CA, 3Division of Nephrology, David Geffen School of Medicine at UCLA, Los Angeles, CA, 4Division of Hematology-Oncology, David Geffen School of Medicine at UCLA, Los Angeles, CA
Meeting: 2019 American Transplant Congress
Abstract number: A168
Keywords: Gene expression, Infection, Kidney transplantation, Rejection
Session Information
Session Name: Poster Session A: Biomarkers, Immune Monitoring and Outcomes
Session Type: Poster Session
Date: Saturday, June 1, 2019
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall C & D
*Purpose: Changes in immune response are central to vulnerability to infection and rejection, especially for the growing numbers of older kidney transplant recipients. We sought to determine whether analysis of changes in gene expression could predict subsequent episodes of infection or rejection.
*Methods: Peripheral blood mononuclear cells were isolated from 24 older (≥ age 60) and 36 matched adult (ages 30-59) kidney transplant recipients at 3 months after transplantation. Older versus younger patients were cohort matched on induction type (basiliximab versus lymphocyte depletion with antithymocyte globulin (ATG) and living versus deceased donor type. Chart review was performed to identify episodes of infection or biopsy-proven acute cellular rejection (ACR) or antibody-mediated rejection (AMR) in the first year after transplantation. RNA extraction was performed on banked PBMCs. Gene expression values from gene array analysis were quantile-normalized and log2-transformed for linear model analyses to identify differential expression as a function of age, adjusted for age, sex, induction type, and donor type (living v. deceased).
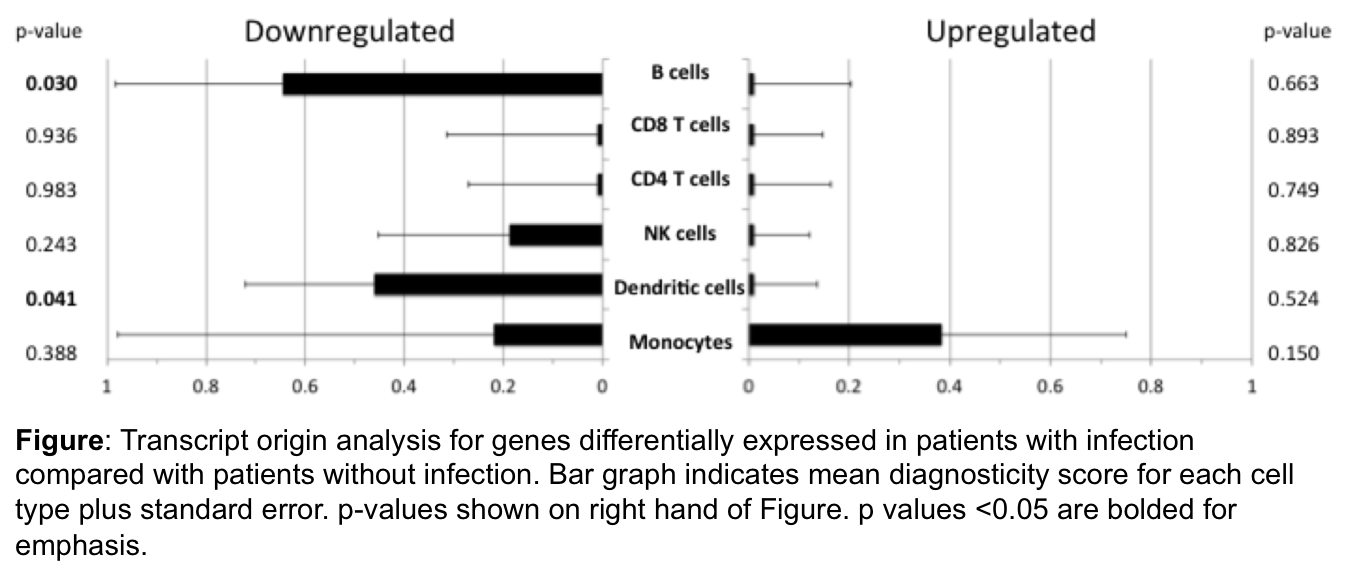
*Results: A variety of pro-inflammatory genes were found to be down-regulated in patients who developed infection after transplantation after correction for age, sex, transplant type, and induction. These included chemokine ligands, cytokines, and HLA Class I molecules. The cell type source for downregulated transcripts were dendritic cells and B cells (Figure). Interestingly, genes involved in iron metabolism and HLA Class II molecules were up-regulated in patients who developed infection. Differentially activated transcription factors included the interferon regulatory factor and IFN-stimulated response element. Patients who developed rejection demonstrated an increase in myeloid lineage immune cell activity.
*Conclusions: Differential patterns of gene expression were observed in patients who developed infection in the first year after kidney transplantation. These findings were distinct from the gene expression changes associated with development of rejection. These findings may explain the mechanism behind vulnerability to infection in older transplant patients. In addition, monitoring of changes in gene expression may provide an avenue for patient monitoring after transplantation as well as individualization of immune suppression after solid organ transplantation.
To cite this abstract in AMA style:
Schaenman J, Rossetti M, Liang E, Beaird OE, Bunnapradist S, Reed EF, Cole S. Transcriptional Changes in PBMC Associated with Development of Infection and Rejection in Older and Younger Kidney Transplant Recipients [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/transcriptional-changes-in-pbmc-associated-with-development-of-infection-and-rejection-in-older-and-younger-kidney-transplant-recipients/. Accessed January 8, 2026.« Back to 2019 American Transplant Congress