Flow Cytometric Analysis of Leukocyte Migration during Ex Vivo Lung Perfusion with CXCR4 Inhibition
1General Surgery, Duke University, Durham, NC, 2Thoracic Surgery, Duke University, Durham, NC
Meeting: 2019 American Transplant Congress
Abstract number: A98
Keywords: Lung, Lung preservation, Perfusion solutions
Session Information
Session Name: Poster Session A: Ischemia Reperfusion & Organ Rehabilition
Session Type: Poster Session
Date: Saturday, June 1, 2019
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall C & D
*Purpose: Ex vivo lung perfusion (EVLP) has emerged as a preservation technique utilized to evaluate candidate donor lungs in a metabolically active state. This also provides a platform for potential allograft reconditioning. Donor leukocytes have been implicated in ischemia reperfusion injury, primary graft dysfunction, and acute rejection. Pharmacologic strategies to enhance donor leukocyte depletion during EVLP have not yet been described. Plerixafor is a clinically available CXCR4 antagonist, blocking the interaction between CXCR4 and SDF-1α. We tested the hypothesis that plerixafor improves donor leukocyte depletion during ex vivo perfusion.
*Methods: The Duke University Institutional Animal Care and Use Committee (IACUC) approved all animal protocols. Rats were housed in standard climate controlled, pathogen free conditions. Heart-lung blocs procured from Lewis rats (225-275g, Charles River) were subjected to 3 hours of normothermic EVLP with Steen Solution (XVIVO) with (N=5) or without (N=6) the addition of plerixafor. Cell counts (cells/μL) were determined using BD Trucount tubes and analyzed using a LSR II flow cytometer (BD Biosciences). Student’s t-test was applied for determination of statistical significance. A probability of less than 0.5 (P <0.05) was considered statistically significant. Statistics were run with GraphPad Prism version 8.
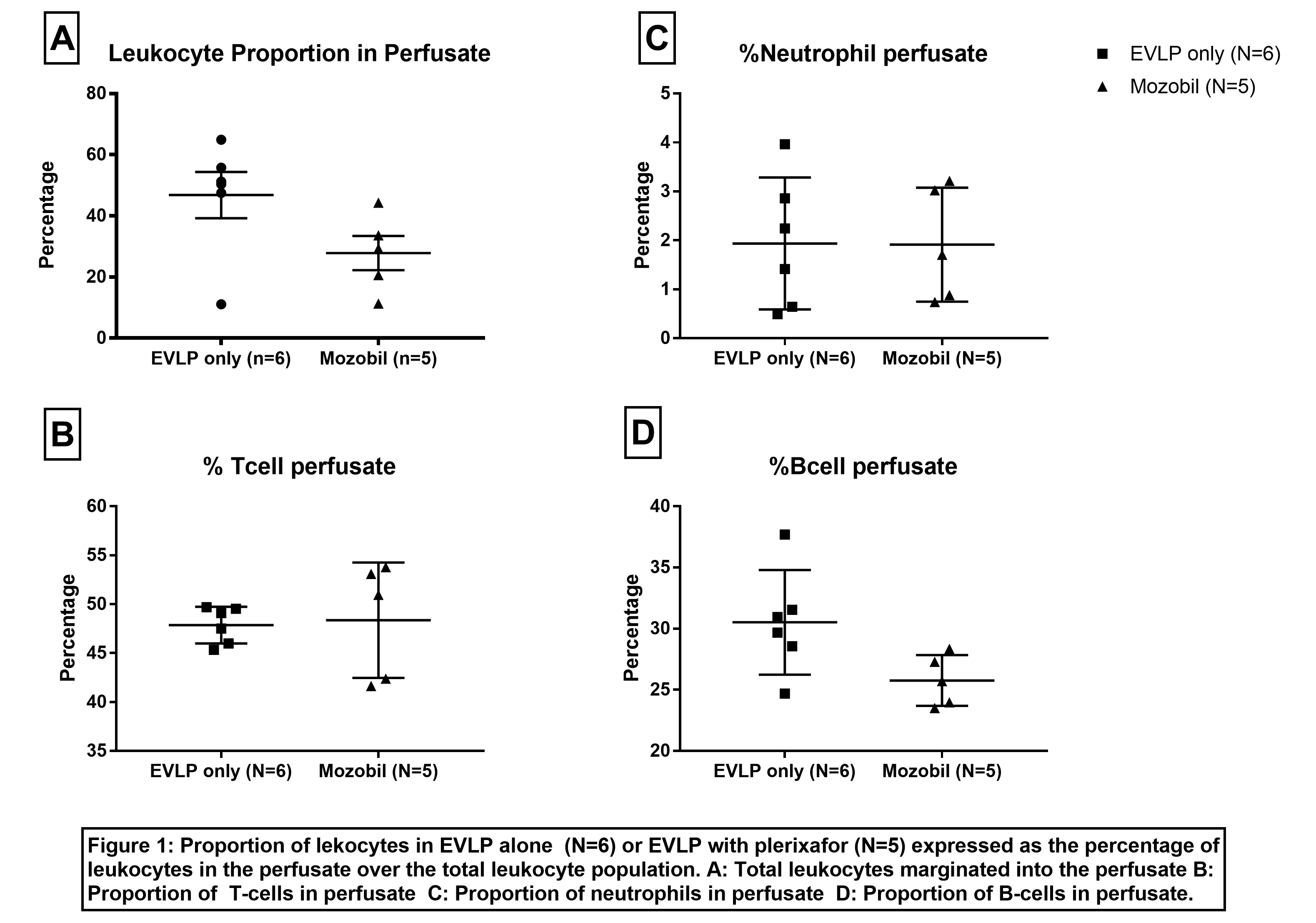
*Results: Leukocytes depleted from the lung during perfusion are expressed as the number of CD45+ cells in the perfusate over the total number of CD45+ cells in the perfusate plus the lung (mean ± SEM). Plerixafor delivered during EVLP (n=5) did not alter leukocyte depletion compared to standard EVLP (n=6) (27.83±5.62% vs. 46.81±7.56%, p=0.084). Proportions of cell populations mobilized into the perfusate were consistent among subjects and groups. Similar proportions of B-cells (25.76±0.93% vs. 30.52±1.74%, p=0.052), T-cells (48.37±2.64% vs. 47.86±0.77%, p=0.845), and neutrophils (1.91±0.52% vs. 1.93±0.55%, p=0.976) were detected in the perfusate regardless of subjects total cell counts or study group (Figure 1). This suggests that flow cytometric analysis was accurate and reproducible for this application.
*Conclusions: Plerixafor does not increase donor leukocyte depletion during EVLP in this rodent model. Flow cytometric analysis of perfusate can provide a novel method of identifying and quantifying specific cell populations during ex vivo perfusion, and will be a useful tool as leukocyte depletion is studied further.
To cite this abstract in AMA style:
Yerxa J, Gao Q, Davis RP, Zhang M, Scheuermann U, Parker W, Hartwig MG, Barbas A. Flow Cytometric Analysis of Leukocyte Migration during Ex Vivo Lung Perfusion with CXCR4 Inhibition [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/flow-cytometric-analysis-of-leukocyte-migration-during-ex-vivo-lung-perfusion-with-cxcr4-inhibition/. Accessed February 5, 2026.« Back to 2019 American Transplant Congress