Ethnic and Age Disparities in Outcomes among Liver Transplant Waitlist Candidates
1University of Alabama at Birmingham, Birmingham
2Department of Veterans Affairs, Washington DC.
Meeting: 2018 American Transplant Congress
Abstract number: C219
Keywords: African-American, Age factors, Liver transplantation, Waiting lists
Session Information
Session Name: Poster Session C: Liver: Recipient Selection
Session Type: Poster Session
Date: Monday, June 4, 2018
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall 4EF
Background: Despite the increasing prevalence of end-stage liver disease (ESLD) in older adults, there is no consensus to determine suitability for liver transplantation (LT) in the elderly. Disparities in LT access exist, with a disproportionately lower percentage of African Americans (AA) receiving LT. Understanding LT waitlist (WL) outcomes in older adults, specifically AA, will identify opportunities to improve LT access for this vulnerable population.
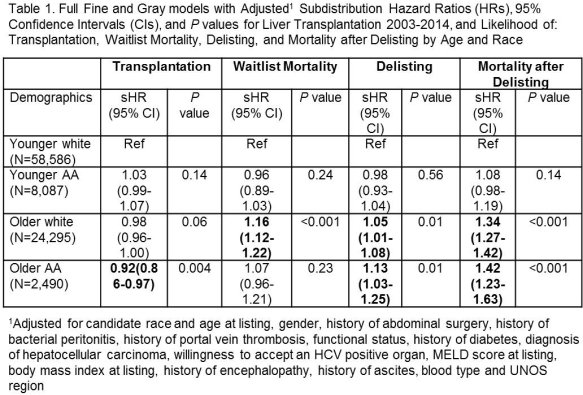
Methods: All adult, liver-only white and AA LT WL candidates (1/1/03-10/1/14) were identified in the Scientific Registry of Transplant Recipients. Age and race categories were defined as younger (age <60) white, younger AA, older (age ≥60) white, and older AA. Outcomes were delisting, transplantation, and WL mortality (supplemented by the Social Security Death Master File and Centers for Medicare and Medicaid Services). To account for underlying age and race differences in LT and WL mortality, outcomes were modeled using Fine and Gray competing risks.
Results: Among 93,458 candidates, 58.1% underwent LT, 14.9% died on the WL, and 20.2% were delisted. Among those delisted, 8.0% were later relisted, and 35.6% died. Outcomes did not differ for younger AA compared with younger whites. However, both older whites (sHR 1.05,95%CI 1.01-1.08) and older AA (sHR 1.13,95%CI 1.03-1.25) were more likely than younger whites to be delisted and to die after delisting (sHR 1.34,95%CI 1.27-1.42 and sHR 1.42,95%CI 1.23-1.63 respectively)(Table). Older whites (sHR 1.16,95%CI 1.12-1.22) were also more likely to die while listed than younger whites. Older AA had no increased risk of WL mortality but were less likely to undergo LT (sHR 0.92, 95%CI 0.86-0.97).
Conclusion: Independent of race, older LT candidates were more likely than younger whites to be delisted and to die after delisting. Older whites had higher WL mortality, while older AA were less likely to undergo LT. Our findings support the need for interventions to ensure medical suitability for LT among older adults and to address disparities in LT access for older AA.
CITATION INFORMATION: Mustian M., Gray S., Shelton B., Reed R., MacLennan P., White J., Eckhoff D., Allman R., Locke J. Ethnic and Age Disparities in Outcomes among Liver Transplant Waitlist Candidates Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Mustian M, Gray S, Shelton B, Reed R, MacLennan P, White J, Eckhoff D, Allman R, Locke J. Ethnic and Age Disparities in Outcomes among Liver Transplant Waitlist Candidates [abstract]. https://atcmeetingabstracts.com/abstract/ethnic-and-age-disparities-in-outcomes-among-liver-transplant-waitlist-candidates/. Accessed February 9, 2026.« Back to 2018 American Transplant Congress