The Impact of Rapamycin Conversion in Pediatric Liver Transplantation on Anti-HLA Antibody Formation and Allograft Fibrosis
1University of Kansas College of Medicine, Kansas City, KS
2Children's Mercy Hospital, Kansas City, MO.
Meeting: 2018 American Transplant Congress
Abstract number: B281
Keywords: HLA antibodies, Immunosuppression, Liver
Session Information
Session Name: Poster Session B: Liver: Pediatrics
Session Type: Poster Session
Date: Sunday, June 3, 2018
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall 4EF
Background: Maintenance immunosuppression with tacrolimus (TAC) is associated with progressive liver allograft fibrosis. Conversion to rapamycin (RAPA) may abrogate this progression. The development of donor-specific anti-human leukocyte antigen antibodies (anti-HLA) may contribute to organ rejection and fibrosis. We compared the impact of conversion from TAC to RAPA on the anti-HLA profile and allograft fibrosis in children.
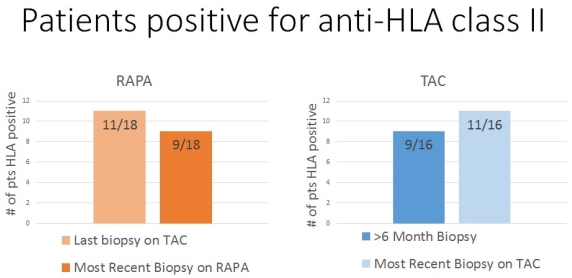
Methods: We retrospectively analyzed the records of 34 patients transplanted between 1994 and 2013. We noted the development and persistence of anti-HLA in patients on maintenance TAC (n= 16) compared to those converted to RAPA (n=18). Patients were categorized by the maintenance immunosuppression at the time of most recent biopsy. We noted anti-HLA at the time of first surveillance biopsy on TAC (~12 months post-transplant), most recent biopsy on TAC and most recent biopsy on RAPA (if applicable). Liver fibrosis was assessed using the METAVIR scoring system. Anti-HLA were considered positive if the mean fluorescence intensity > 1000.
Results: Only one patient in each group was positive for class I anti-HLA on most recent biopsy. Of the 18 patients converted to RAPA, 2 of 11 patients that were class II anti-HLA on TAC became anti-HLA negative on RAPA. Of the 16 patients maintained on TAC, 9 were class II anti-HLA positive on their first surveillance biopsy, and 11 were positive on their most recent biopsy on TAC (see figure). One RAPA patient lost DQ anti-HLA, and another lost the DQ, DR, and DP serotypes. One TAC patient lost DQ anti-HLA, while two acquired DQ, DR and DP serotypes and one acquired DR anti-HLA. Patients on RAPA showed reduced fibrosis in 39% of patients, including the two patients that lost anti-HLA.
Conclusion: These data suggest RAPA maintenance therapy may inhibit anti-HLA development in pediatric liver transplant patients and may contribute to decreased allograft fibrosis. Further evaluation of larger patient populations is indicated.
CITATION INFORMATION: Fischer R., Fromm L., Daniel J., Kats A., Hendrickson R., Andrews W. The Impact of Rapamycin Conversion in Pediatric Liver Transplantation on Anti-HLA Antibody Formation and Allograft Fibrosis Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Fischer R, Fromm L, Daniel J, Kats A, Hendrickson R, Andrews W. The Impact of Rapamycin Conversion in Pediatric Liver Transplantation on Anti-HLA Antibody Formation and Allograft Fibrosis [abstract]. https://atcmeetingabstracts.com/abstract/the-impact-of-rapamycin-conversion-in-pediatric-liver-transplantation-on-anti-hla-antibody-formation-and-allograft-fibrosis/. Accessed February 20, 2026.« Back to 2018 American Transplant Congress