Living Kidney Transplant: The Influence of Intraoperative Hemodynamics on Delayed Graft Function.
1Scripps Center for Organ and Cell Transplantation, Scripps Green Hospital, La Jolla, CA
2Research Department and Analytics, UNOS, Richmond, VA
Meeting: 2017 American Transplant Congress
Abstract number: A249
Keywords: Graft survival, Outcome, Renal ischemia, Risk factors
Session Information
Session Name: Poster Session A: Living Donor Kidney Transplant I
Session Type: Poster Session
Date: Saturday, April 29, 2017
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall D1
Despite advantages of living donor kidneys, intraoperative insults may subject these kidneys to poor outcomes. Therefore, we investigated whether intraoperative fluid volumes and hemodynamics in the donor, and recipient, could act as predictors of delayed graft function (DGF) and subsequent outcomes.
Methods: All living kidney donors and recipients from 2010-2016 at this institution underwent a retrospective chart review. Graft function in the first week after transplant was used to group recipients into DGF (need for dialysis), slow graft function (SGF) (creatinine >2.5) and good function (GF) cohorts. Groups were analyzed for differences between intraoperative fluid totals and hemodynamics. At 1 year, incidence of acute rejection, graft function, survival and biopsy results were compared. Chi-squared test was used for categorical variables and Kruskal-Wallis test for continuous variables.
Results: A total of 111 living renal transplants were performed. 53% and 47% of recipients were male and female respectively. 2.7% (n=3) and 15% (n=17) developed DGF and SGF respectively. All DGF cases were in males, while being female was associated with GF (p=0.006). Pre-operative hemodialysis was associated with DGF and SGF (p=0.014). DGF was associated with greater donor height, weight and BSA (p=0.011 / 0.009 / 0.047). Minimum recipient central venous pressure over 12mmHg was associated with DGF (p=0.003), while intraoperative hypotension (systolic <90mmHg or diastolic <50mmHg) was not. In the recipient and donor, fluid volumes and EBL did not differ amongst groups. DGF had a higher incidence of rejection than GF (33% vs 3%, p=0.016). Tubular atrophy on 1 year biopsy was associated with SGF (p=0.034). All groups had similar 1 year graft function & survival.
Conclusions: This single center retrospective review suggests that larger donors and CVP greater that 14mmHg is associated with DGF, despite no association with an incident of hypotension. There was a trend towards tubular atrophy with SGF. Despite this, 1 year graft function and survival was equivalent.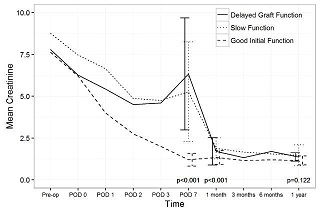
CITATION INFORMATION: Schutt R, Case J, Barrick B, Toll A, Marsh C. Living Kidney Transplant: The Influence of Intraoperative Hemodynamics on Delayed Graft Function. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Schutt R, Case J, Barrick B, Toll A, Marsh C. Living Kidney Transplant: The Influence of Intraoperative Hemodynamics on Delayed Graft Function. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/living-kidney-transplant-the-influence-of-intraoperative-hemodynamics-on-delayed-graft-function/. Accessed February 19, 2026.« Back to 2017 American Transplant Congress
