Blood Transfusion Before Organ Transplant: Patient Sensitization and Outcomes.
Laboratory Medicine and Pathology, University of Minnesota, Minneapolis, MN
Meeting: 2017 American Transplant Congress
Abstract number: A27
Keywords: Blood transfusion, HLA antibodies, Sensitization
Session Information
Session Name: Poster Session A: Antibody Mediated Rejection in Kidney Transplant Recipients I
Session Type: Poster Session
Date: Saturday, April 29, 2017
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall D1
Background
Blood transfusions (Btf) can cause alloimmunization to HLA antigens. Antibodies to HLA (HLAb) can increase patients' calculated panel reactive assay (cPRA) and make it more difficult to find compatible donor organs. However, the magnitude of the effects of Btf on organ transplant outcomes is not known.
Methods
We retrospectively studied 92 patients who received Btf prior to kidney (n=34), lung (n=8), or heart transplant (n=50) at our institution between December 2009 and June 2016. We measured HLAb levels, using a single antigen bead assay, in samples obtained before and up to 3-months after Btf. A significant HLAb was defined based on mean fluorescence index (MFI) using two thresholds: high threshold, MFI >3000; and low threshold, MFI >500. Then, patients were grouped as having an increase or no increase in the number of HLAb after transfusion. These groups were compared for post-transplant 1-year survival and 1-year rejection-free survival.
Results
24% of patients (n=22) developed at least one additional high threshold HLAb, and more than 50% of patients (n=51) developed at least one new low threshold HLAb in the first 3 months after Btf. 1-year survival in all groups was greater than 90% and there was no significant difference in patients that had an increased number of HLAb vs. no increase (high threshold: P=0.937, low threshold: P=0.505). 41 patients were treated for rejection (biopsy proven in 32 patients) within the first year after transplant. 1-year rejection-free survival was significantly worse in patients with an increased number of high threshold HLAb (31% vs 70%, P=0.033; Fig. 1A), but not in those that had an increased number of low threshold HLAb (63% vs. 57%, P=0.918; Fig. 1B).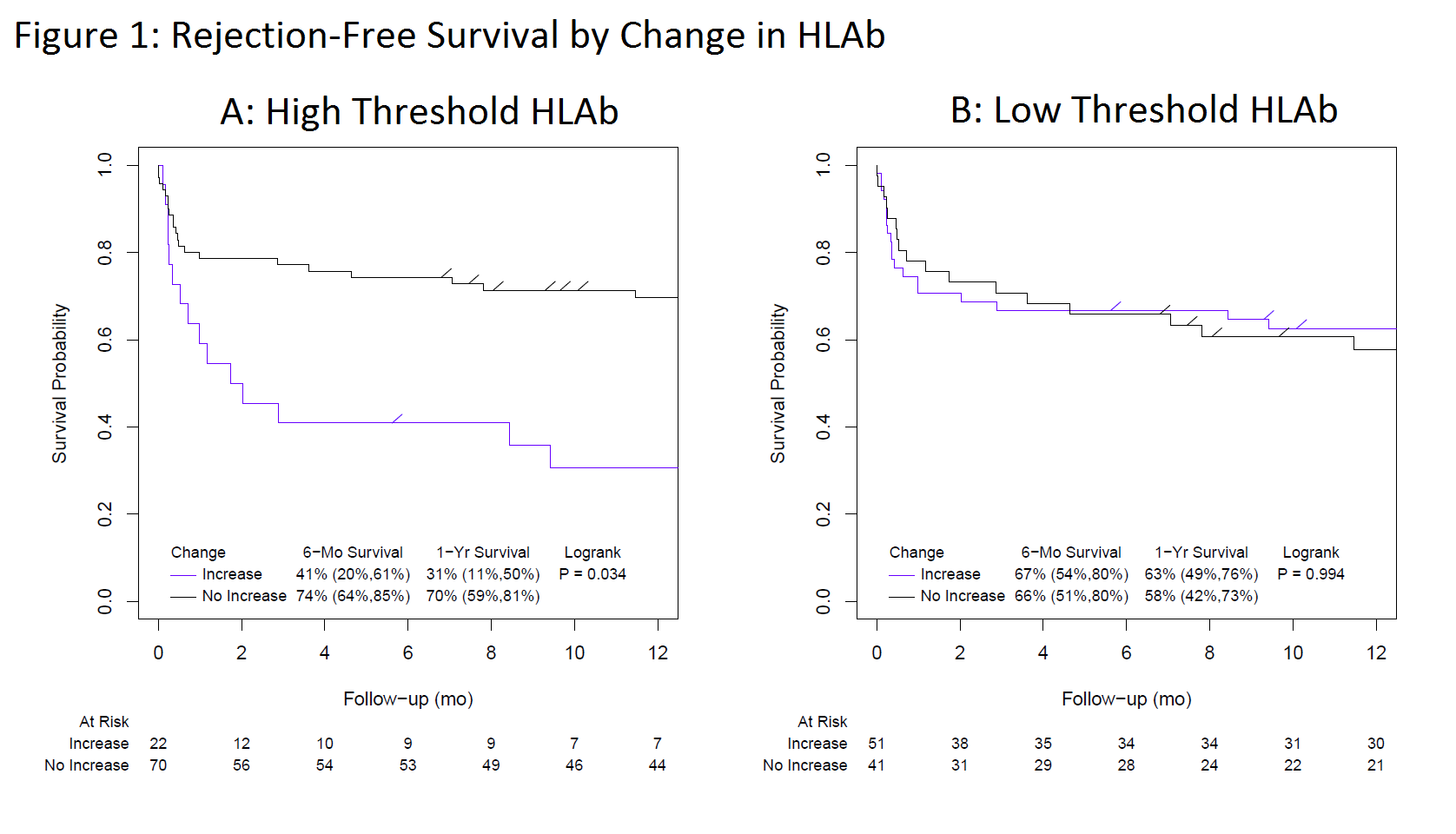 Conclusion
Conclusion
A large proportion of patients transfused while on the wait list had an increase in HLAb. There was no difference in 1-year post-transplant mortality risk in patients that did or did not have an increase in HLAb. However, patients that developed HLAb with MFI>3000 had a greater risk of treatment for rejection within the first post-transplant year.
CITATION INFORMATION: Cich I, Rudser K, Brown R, Ibrahim H, Thorson R, Patil J, Loor G, Hertz M, Cohn C. Blood Transfusion Before Organ Transplant: Patient Sensitization and Outcomes. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Cich I, Rudser K, Brown R, Ibrahim H, Thorson R, Patil J, Loor G, Hertz M, Cohn C. Blood Transfusion Before Organ Transplant: Patient Sensitization and Outcomes. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/blood-transfusion-before-organ-transplant-patient-sensitization-and-outcomes/. Accessed February 24, 2026.« Back to 2017 American Transplant Congress
