Primary Graft Dysfunction After Pediatric Heart Transplant.
Pediatric Cardiology, Washington University School of Medicine, St. Louis, MO
Meeting: 2017 American Transplant Congress
Abstract number: 224
Keywords: Graft failure, Graft function, Heart transplant patients, Pediatric
Session Information
Session Name: Concurrent Session: Heart Transplantation: Antibodies and Outcomes
Session Type: Concurrent Session
Date: Monday, May 1, 2017
Session Time: 2:30pm-4:00pm
 Presentation Time: 3:30pm-3:42pm
Presentation Time: 3:30pm-3:42pm
Location: E271b
Background: Primary graft dysfunction (PGD), as defined by ISHLT Consensus Guidelines, has been associated with worse outcomes in adult heart transplant recipients, even in patients who do not require mechanical support. This is not an established risk factor in the pediatric population. We aim to define the incidence of PGD, and impact on clinical outcomes,in a pediatric heart transplant population.
Methods: We applied adult ISHLT PGD consensus guidelines, which include number and doses of inotropes and need for mechanical circulatory support (MCS), to 208 pediatric OHT recipients from Jan 2005-May 2016. PGD was defined as: moderate PGD – inotrope score >10 on post-operative day 1 (24-48 hours), and severe PGD – MCS within 24 hours (in the absence of rejection).
Results: PGD occurred in 36 patients (17%); 18 of which had severe PGD (8.5%). All with severe PGD were on ECMO. Multivariate risk factors for PGD included a positive cross match (PCM) (OR 7.23, 95% 1.9,29.8, p<0.01) and cardiopulmonary bypass time (CPBT) (OR 10.14/10 min, 95% 10.05,10.2, p<0.01), but not age, weight, ischemic time, or primary diagnosis. Risk factors for severe PGD also included PCM (OR 7.87, 95% 1.26,55.4, p=0.03) and CPBT (OR 10.3/10 min, 95% 10.05,10.2, p=0.03). Patients with PGD vs those without PGD, had longer hospital courses (28 vs 10 days (med), p<0.01); yet when comparing patients with moderate PGD to without PGD, they also had longer courses (26 vs 10 days) but this was not statistically significant (p=0.08). Patients with PGD had decreased overall survival (69% vs 85%, p=0.03), which remained significant on multivariate analysis (HR 2.82, 95% CI 1.01, 7.67, p<0.01 ). Severe PGD was associated with the worst survival; yet survival was comparable between moderate PGD and those without PGD (89% vs 85%, p=0.65).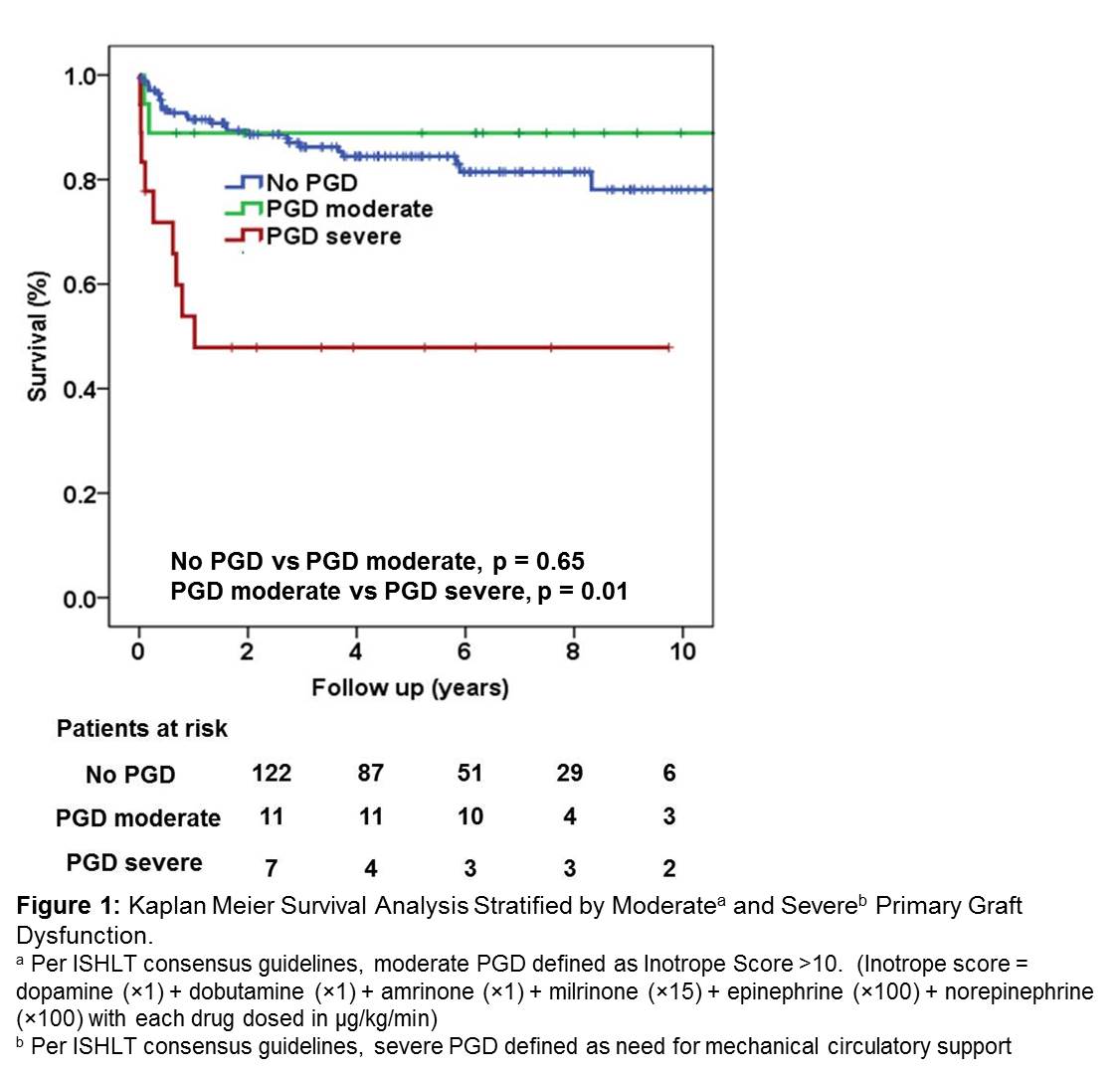 Conclusion: In the current era, infants do not have increased risk of PGD; however it appears to be related to CPBT and PCM. Need for MCS, but not high dose inotropes, is associated with increased mortality. The association of PCM and severe PGD in the absence of detectable rejection requires further investigation.
Conclusion: In the current era, infants do not have increased risk of PGD; however it appears to be related to CPBT and PCM. Need for MCS, but not high dose inotropes, is associated with increased mortality. The association of PCM and severe PGD in the absence of detectable rejection requires further investigation.
CITATION INFORMATION: Mowers K, Simpson K, Eghtesady P, Petrucci O, Canter C, Castleberry C. Primary Graft Dysfunction After Pediatric Heart Transplant. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Mowers K, Simpson K, Eghtesady P, Petrucci O, Canter C, Castleberry C. Primary Graft Dysfunction After Pediatric Heart Transplant. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/primary-graft-dysfunction-after-pediatric-heart-transplant/. Accessed February 12, 2026.« Back to 2017 American Transplant Congress
