Acute Inflammation, Chronic Damage and Renal Dysfunction in Renal Transplant Recipients with Delayed Graft Function (DGF).
UPMC, Pittsburgh.
Meeting: 2016 American Transplant Congress
Abstract number: 99
Keywords: Graft function, Inflammation
Session Information
Session Name: Concurrent Session: Delayed Graft Function and Protocol Biopsy
Session Type: Concurrent Session
Date: Sunday, June 12, 2016
Session Time: 4:30pm-6:00pm
 Presentation Time: 4:54pm-5:06pm
Presentation Time: 4:54pm-5:06pm
Location: Room 302
Analysis of DGF and clinical outcomes in relation to progressive histological changes is not well reported. In this prospective longitudinal study, patients with DGF were compared to those with Primary Graft Function (PGF) for changes in renal function as well as acute and chronic histological lesions in the first post-Tx year through protocol (3m & 12m) and for-cause biopsies.
370 patients who were transplanted between 1/13-11/14 were prospectively studied (Thymo with MPA-TAC & rapid steroid withdrawal). 72 patients (19.5%) had DGF and were compared to those with PGF (with a further analysis of LD & DD Txs). Patient demographics including KDPI scores were comparable. 29/79(36%) patients with DGF>2wks were biopsied for renal dysfunction.
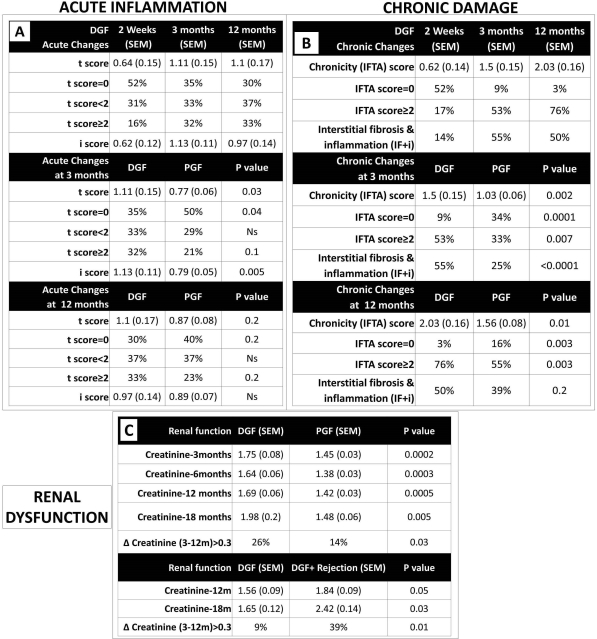
Acute Inflammation: Significant tubulointerstitial inflammation (TI) was noted in the DGF group at 2wks that persisted at 3m and 12m. Patients with DGF had significantly more TI at 3m compared to those with PGF with a similar trend at 12m (Fig-1A). These findings translated to 60% clinical/subclinical T cell rejection in the DGF group in comparison to 37% in those with PGF (P<0.05).
Chronic damage: Chronic damage (IFTA, IF+i) was worse at 3 and 12m in the DGF group compared to PGF (Fig-1B). Importantly 50% of those with DGF had chronic damage (mild-moderate IFTA and IF+i) as early as 3m(Fig-1B). In patients with DGF, chronic damage was minimal at 2 weeks, however, progressed significantly at 3 and 12m. Patients who experienced a DGF and rejection had the greatest degree of chronic damage.
Renal Function: Patients with DGF had significantly worse creatinine at 3, 6, 12 and 18m with a significantly higher proportion of patients showing progressive dysfunction ([Delta] creatinine 3-12m>0.3) (Fig-1C). Within the DGF group, patients who experienced a rejection episode had the worst renal function (Fig-1C).
All the above results remained unchanged when the analysis was repeated in DD and LD Txs separately.
To conclude, in patients with DGF, early allograft perfusion injury coupled with TI leads to early progressive chronic allograft damage and renal dysfunction. Thus events early after transplant determine allograft injury impacting graft outcomes.
CITATION INFORMATION: Cherukuri A, Mehta R, Sood P, Randhawa P, Tevar A, Hariharan S. Acute Inflammation, Chronic Damage and Renal Dysfunction in Renal Transplant Recipients with Delayed Graft Function (DGF). Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Cherukuri A, Mehta R, Sood P, Randhawa P, Tevar A, Hariharan S. Acute Inflammation, Chronic Damage and Renal Dysfunction in Renal Transplant Recipients with Delayed Graft Function (DGF). [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/acute-inflammation-chronic-damage-and-renal-dysfunction-in-renal-transplant-recipients-with-delayed-graft-function-dgf/. Accessed February 27, 2026.« Back to 2016 American Transplant Congress
